To maximize the benefits of Zithromax, understanding its spectrum of action against various pathogens is key. Zithromax, or azithromycin, primarily targets gram-positive bacteria, but its effectiveness extends to certain gram-negative organisms and atypical pathogens. This broad spectrum makes it a valuable option for treating infections such as community-acquired pneumonia and various skin infections.
While Zithromax excels against Streptococcus pneumoniae and Staphylococcus aureus, it also inhibits the growth of Mycoplasma pneumoniae and Chlamydia pneumoniae. This versatility means many patients can find relief from respiratory and sexually transmitted infections with a single medication.
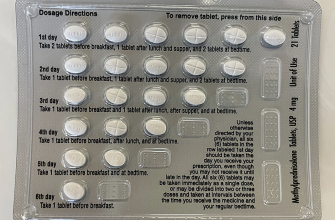
Consider dosage adjustments based on the severity of the infection and patient factors. For respiratory infections, a common regime involves a loading dose, followed by a shorter course, which can enhance compliance and reduce side effects. Always consult healthcare providers for personalized recommendations to ensure optimal treatment outcomes.
- Zithromax Spectrum: A Comprehensive Overview
- Understanding the Mechanism of Action of Zithromax
- Clinical Applications and Indications for Zithromax Use
- Common Indications
- Special Considerations
- Potential Side Effects and Drug Interactions to Consider
- Resistance Patterns and the Future of Zithromax Therapy
- Current Resistance Trends
- Future Implications for Therapy
Zithromax Spectrum: A Comprehensive Overview
Zithromax, known by its generic name azithromycin, exhibits a wide range of activity against various pathogens. This macrolide antibiotic is renowned for its effectiveness against respiratory infections, skin infections, and sexually transmitted diseases.
The primary spectrum of Zithromax includes gram-positive bacteria, notably Streptococcus pneumoniae and Staphylococcus aureus. It also tackles notable gram-negative bacteria, such as Haemophilus influenzae and Moraxella catarrhalis. Zithromax has gained recognition for its action against atypical pathogens, including Mycoplasma pneumoniae and Chlamydia pneumoniae, making it a valuable option for atypical pneumonia treatment.
The pharmacokinetics of Zithromax contribute to its appeal. A single dose achieves extensive tissue penetration, allowing for sustained antimicrobial activity. This long half-life permits shorter treatment courses, often just three to five days, compared to traditional antibiotics requiring longer regimens.
Indications for Zithromax expand beyond typical applications. It is prescribed for community-acquired pneumonia, sinusitis, bronchitis, and even as part of a regimen for Helicobacter pylori eradication. Its use in the treatment of STIs is also well-documented, particularly in cases of chlamydia and gonorrhea.
Possible side effects include gastrointestinal disturbances like nausea and diarrhea, although these are generally mild. Healthcare providers should monitor for allergic reactions and potential interactions with other medications, especially in patients with underlying health conditions.
Resistance patterns have emerged over time, making it critical for clinicians to consider local susceptibility data. Employing Zithromax judiciously can help mitigate resistance development and preserve its efficacy.
In conclusion, Zithromax remains a versatile antibiotic with a robust spectrum of activity against a variety of infectious agents. Its pharmacokinetic advantages and broad application make it a staple in many therapeutic protocols. Careful consideration of its use is essential for optimizing treatment outcomes and combating potential resistance.
Understanding the Mechanism of Action of Zithromax
Zithromax, or azithromycin, targets bacterial infections through a specific mechanism of action that disrupts protein synthesis. It binds to the 50S ribosomal subunit of susceptible bacteria, inhibiting the translocation process during protein synthesis. This action ultimately results in the inhibition of bacterial growth and replication.
Here’s a breakdown of the mechanism:
- Binding Site: Azithromycin attaches to the 23S rRNA component of the 50S ribosomal subunit.
- Disruption of Translation: By binding, it obstructs the exit tunnel of the ribosome. This blockage prevents the formation of peptide bonds.
- Inhibition of Protein Formation: Without proper protein synthesis, bacteria cannot grow or reproduce effectively, leading to bacterial cell death.
Zithromax demonstrates activity against a wide variety of pathogens, including:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Mycoplasma pneumoniae
- Chlamydia trachomatis
This broad-spectrum activity makes azithromycin a popular choice for treating various infections, including respiratory tract infections, skin infections, and sexually transmitted diseases. Its pharmacokinetic properties also enhance its effectiveness:
- High tissue penetration: It accumulates in tissues, allowing prolonged action against pathogens.
- Long half-life: This feature supports a convenient dosing schedule, often allowing for a short treatment course.
In summary, Zithromax effectively combats bacterial infections through targeted inhibition of protein synthesis, demonstrating its utility in treating a range of infectious diseases.
Clinical Applications and Indications for Zithromax Use
Zithromax, known generically as azithromycin, serves as a broad-spectrum antibiotic frequently prescribed for various bacterial infections. It particularly targets respiratory tract infections, skin infections, and certain sexually transmitted diseases. This medication’s capability to inhibit bacterial protein synthesis makes it effective against susceptible organisms.
Common Indications
For upper respiratory infections such as sinusitis, Zithromax is often the preferred option due to its efficacy and ease of administration. Additionally, it is indicated for acute bronchitis when a bacterial cause is suspected. In cases of community-acquired pneumonia, especially in patients with allergies to beta-lactams, Zithromax provides a viable alternative.
Skin and soft tissue infections pose another area where Zithromax is frequently utilized. It proves effective against organisms like Staphylococcus aureus and Streptococcus pyogenes, contributing to successful treatment outcomes. Chlamydia trachomatis infections, commonly associated with urethritis and cervicitis, are effectively addressed with Zithromax in a single-dose regimen.
Special Considerations
In pediatric populations, Zithromax demonstrates safety and effectiveness for treating otitis media and pharyngitis. Prescribers often select this antibiotic due to its palatable oral formulation, which aids adherence. It’s important to note that Zithromax is contraindicated in patients with known hypersensitivity to macrolides.
Clinicians should remain vigilant regarding potential drug interactions, particularly with medications that inhibit hepatic metabolism. Regular assessment of patient history ensures optimal therapeutic outcomes while minimizing adverse effects. The appropriate use of Zithromax enhances treatment efficacy and contributes to combating resistant bacterial strains.
Potential Side Effects and Drug Interactions to Consider
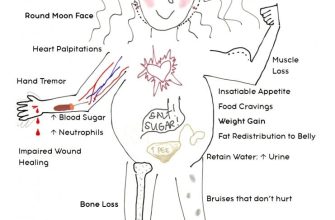
Zithromax may cause side effects such as gastrointestinal disturbances, including nausea, vomiting, diarrhea, and abdominal pain. A skin rash or allergic reactions, including itching or swelling, can occur in some individuals.
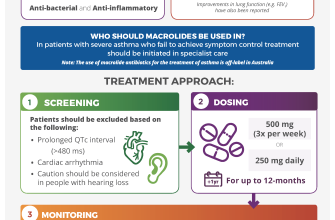
Cardiovascular effects like QT prolongation may arise, especially in patients with existing heart conditions. Monitoring is advised for those with a history of arrhythmias.
Drug interactions can modify the effectiveness of Zithromax or increase the risk of adverse effects. Antacids containing aluminum or magnesium should not be taken within two hours of Zithromax, as they can reduce its absorption.
Concurrent use of anticoagulants, such as warfarin, may enhance the anticoagulant effect, necessitating closer monitoring of INR levels. Consult your healthcare provider if you are taking medications for heart rhythm disturbances, as certain drugs can interact negatively with Zithromax.
Your healthcare provider can offer tailored guidance to manage potential side effects and interactions effectively.
Resistance Patterns and the Future of Zithromax Therapy
Monitoring resistance patterns is critical for the effective use of Zithromax (azithromycin). Studies reveal rising resistance among common pathogens, particularly within Streptococcus pneumoniae and Neisseria gonorrhoeae. This resistance impacts the efficacy of Zithromax, necessitating regular surveillance to guide treatment decisions.
Current Resistance Trends
In recent years, resistance to Zithromax has increased significantly. Data indicates that approximately 30% of Streptococcus pneumoniae strains exhibit resistance. Similarly, Neisseria gonorrhoeae shows alarming trends, with over 50% of strains demonstrating decreased susceptibility. Practitioners should consider these statistics when prescribing Zithromax, especially for community-acquired infections.
Future Implications for Therapy
Enhancing susceptibility testing will play a key role in managing resistance. Clinicians must utilize rapid testing methods to identify resistance before prescribing Zithromax, ensuring targeted therapy. Developing new formulations or alternatives may be necessary to combat increasing resistance. Ongoing research into combination therapies could offer additional strategies to improve outcomes in resistant infections.