The recommended duration of azithromycin therapy typically ranges from three to seven days, depending on the type of infection being treated. For acute bacterial sinusitis, a five to seven-day course is suggested. In the case of bacterial pneumonia, three days of treatment often suffice, with clinical improvement observed within this timeframe.
Patients receiving azithromycin for chlamydia should adhere to a single dose of 1 gram, while those treated for uncomplicated skin infections may require a five-day course. It’s important to follow these durations closely to enhance recovery and prevent resistance. Monitoring of symptoms during treatment is essential to assess effectiveness.
Adjustments to therapy duration may be necessary based on individual response and the presence of any underlying conditions. Always consult with a healthcare professional for personalized recommendations to ensure optimal treatment outcomes.
- Azithromycin Duration of Therapy
- Understanding Azithromycin: Mechanism of Action
- Key Mechanisms
- Application and Dosing
- Recommended Duration for Common Infections
- Skin Infections
- Chlamydia Infections
- Factors Influencing Treatment Duration
- Comparison with Other Macrolide Antibiotics
- Dosing Differences
- Tolerability and Side Effects
- Potential Side Effects of Prolonged Use
- Common Side Effects
- Serious Concerns
- Patient Adherence and Treatment Outcome
- Future Directions in Azithromycin Therapy Research
Azithromycin Duration of Therapy
For most bacterial infections treated with azithromycin, the typical duration of therapy ranges from 3 to 7 days. For community-acquired pneumonia, a common indication, a 5-day course is frequently recommended. In cases of uncomplicated bacterial sinusitis, a 3-day regimen may suffice.
Patients with chlamydia infections generally benefit from a single, high-dose administration of 1 gram. For skin and soft tissue infections, the duration may extend to 7 days, depending on the severity and type of infection.
Adherence to the prescribed duration is crucial. Shortening the treatment period can lead to incomplete eradication of the infection, potentially resulting in relapse or resistance. Always consult a healthcare professional to determine the appropriate duration based on individual circumstances.
In pediatric cases, azithromycin is often used for acute otitis media, where a 5-day course is common. Adjustments in dosage may be necessary based on the child’s weight and specific health conditions.
Monitor for side effects during treatment. While generally well-tolerated, gastrointestinal disturbances can occur. If severe reactions arise, seek medical advice promptly.
Understanding Azithromycin: Mechanism of Action
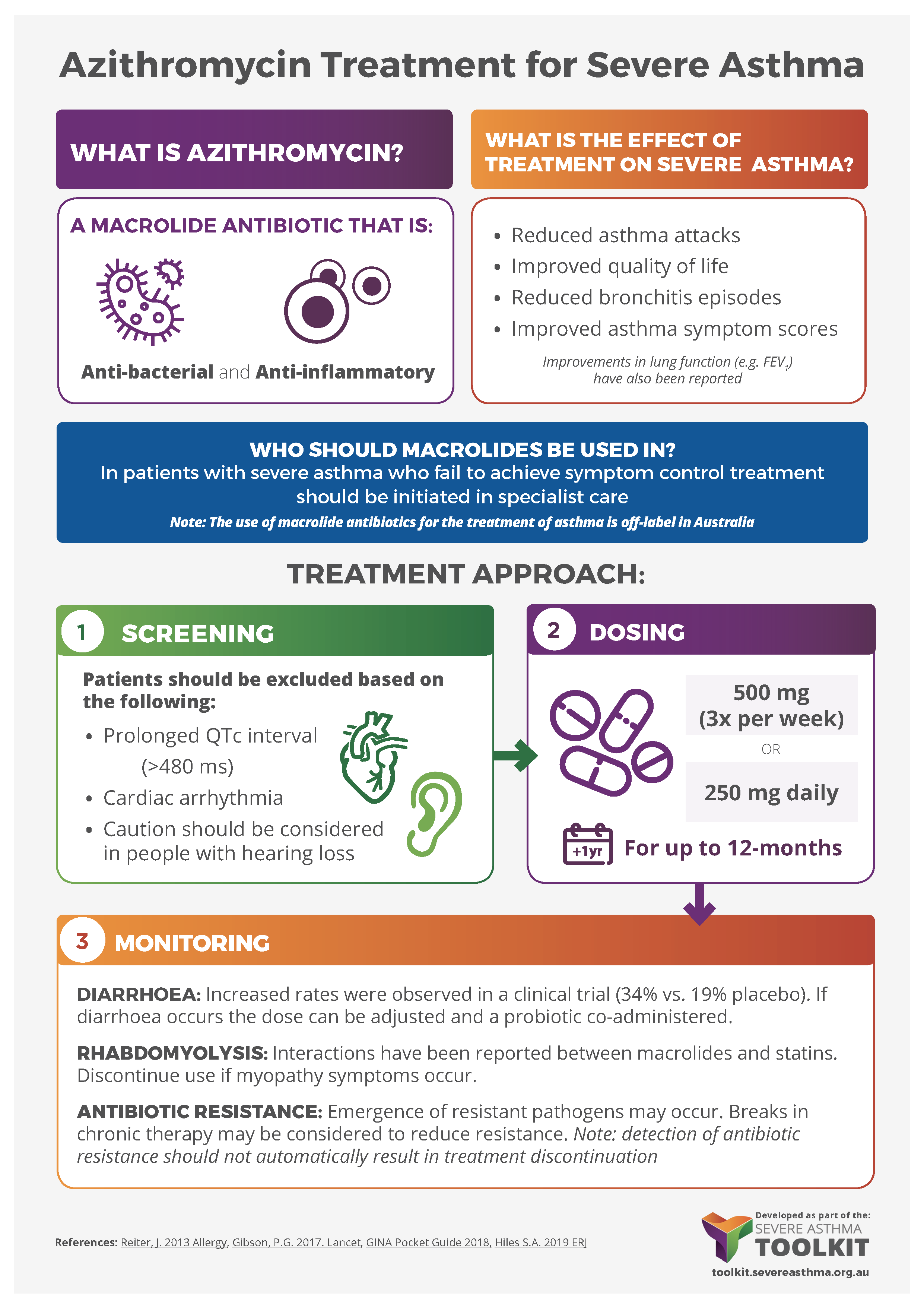
Azithromycin works by inhibiting bacterial protein synthesis. It binds to the 50S subunit of the bacterial ribosome, obstructing the translation process necessary for protein formation. This action halts bacterial growth and reproduction, facilitating the immune system in eradicating the infection.
Key Mechanisms
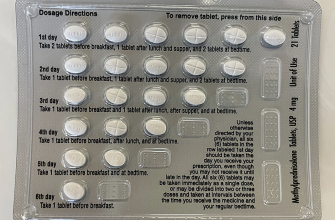
- Time-dependent killing: The effectiveness of azithromycin increases with the duration the drug remains above the minimum inhibitory concentration (MIC). Dosing regimens often include a loading dose followed by a shorter duration for optimal results.
- Broad-spectrum activity: Azithromycin targets a wide range of Gram-positive and Gram-negative bacteria, making it versatile for treating various infections such as respiratory and skin infections.
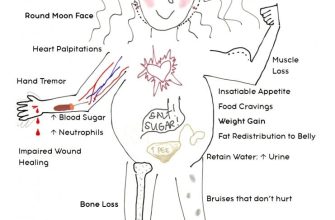
- Anti-inflammatory properties: Beyond its antibacterial action, azithromycin reduces inflammation, which aids in conditions like asthma and chronic obstructive pulmonary disease (COPD).
Application and Dosing
For effective treatment, follow the prescribed dosing schedule. Typical regimens may include a 5-day course for respiratory infections or a single large dose for certain sexually transmitted infections. Always consult a healthcare provider for tailored advice based on the specific infection and individual patient factors.
Understanding the mechanism of action aids in appreciating why azithromycin is a preferred antibiotic in many scenarios. This knowledge also supports informed decisions regarding its application and expected outcomes during therapy.
Recommended Duration for Common Infections
For streptococcal pharyngitis, a course of azithromycin for 5 days is effective. This duration ensures sufficient bacterial eradication and symptom relief.
In the case of community-acquired pneumonia, a treatment plan of 5 to 7 days is recommended. For patients with mild to moderate infections, adherence to this timeframe usually leads to positive outcomes.
Skin Infections
For uncomplicated skin and soft tissue infections, a 5-day regimen suffices. Azithromycin helps in controlling the infection and aiding recovery within this period.
Chlamydia Infections
For Chlamydia trachomatis, a single dose of azithromycin (1 gram orally) is sufficient. This approach provides rapid treatment and supports high cure rates.
Factors Influencing Treatment Duration
The duration of azithromycin therapy typically ranges from 3 to 14 days, depending on various factors. Key considerations include the type of infection, the patient’s age, and presence of co-existing medical conditions. For respiratory infections, a 5-day course is often sufficient, while more severe infections may require longer treatment.
Microbial resistance also plays a significant role in determining treatment length. In cases where resistant strains are suspected, clinicians might extend therapy or consider alternative medications. Regular susceptibility testing can help guide effective treatment duration.
Patient adherence influences the overall effectiveness of therapy. If adherence is poor, extending treatment duration may be necessary to ensure complete resolution of the infection. Educating patients about the importance of finishing their prescribed course enhances adherence rates.
Table 1 outlines common conditions treated with azithromycin and their recommended treatment duration:
| Condition | Recommended Duration |
|---|---|
| Community-acquired pneumonia | 5-7 days |
| Sinusitis | 3 days |
| Skin infections | 7-14 days |
| Chlamydia infections | 1 day (single dose) |
| Gonorrhea | 1 day (single dose) |
Age also affects treatment duration. Older adults may require longer courses due to slower metabolism and potential drug interactions. Pediatric dosing should be carefully monitored to avoid complications and ensure safety.
Finally, individual patient response is crucial. If symptoms persist despite treatment, it may indicate an inadequate response, warranting a reassessment of diagnosis and possible extension of therapy.
Comparison with Other Macrolide Antibiotics
Azithromycin is often compared with other macrolide antibiotics such as clarithromycin and erythromycin regarding dosage, duration of therapy, and spectrum of activity. Azithromycin typically requires a shorter treatment duration, often just five days for respiratory infections, while clarithromycin and erythromycin may necessitate longer courses, ranging from 7 to 14 days.
Clarithromycin shares a similar spectrum of activity as azithromycin but may pose a higher risk of drug interactions due to its potential to inhibit cytochrome P450 enzymes. Clinicians prefer azithromycin in patients taking multiple medications, decreasing the likelihood of adverse reactions.
Dosing Differences
The dosing regimens of these antibiotics vary. Azithromycin’s extended half-life allows for once-daily dosing–a significant convenience over clarithromycin and erythromycin, which often require multiple doses per day. This factor enhances patient adherence to the treatment regimen.
Tolerability and Side Effects
In terms of tolerability, azithromycin generally has a favorable profile. While all macrolides can cause gastrointestinal side effects, azithromycin is often better tolerated, allowing for more consistent completion of therapy. It also boasts a lower incidence of certain side effects, such as QT prolongation, compared to erythromycin.
When selecting a macrolide antibiotic, consider the infection type, patient-specific factors, and potential interactions with other medications. Azithromycin stands out with its shorter treatment duration and ease of dosing, presenting a reliable option for effective patient management.
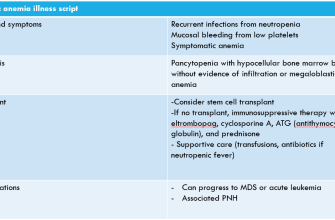
Potential Side Effects of Prolonged Use
Prolonged use of azithromycin can lead to several side effects that warrant attention. Regular monitoring is vital to ensure patient safety and treatment efficacy.
Common Side Effects
- Gastrointestinal Issues: Nausea, diarrhea, and abdominal pain are frequently reported. Reducing the dose or administering with food can help alleviate these symptoms.
- Headaches: Persistent headaches may occur. Staying hydrated and rest can mitigate this effect.
- Skin Reactions: Rashes or itching can develop. Discontinuing the medication may be necessary if these symptoms persist.
Serious Concerns
- Cardiac Effects: Prolonged use can increase the risk of QT prolongation, potentially leading to serious heart rhythm disturbances. Regular ECG monitoring is recommended, particularly in patients with pre-existing heart conditions.
- Liver Function: Extended therapy might affect liver enzymes. Routine blood tests can help track liver function and detect any abnormalities early on.
- Antibiotic Resistance: Long-term use raises the risk of developing resistance. It’s essential to conduct cultures and sensitivity testing before initiating azithromycin therapy.
Patients on long-term azithromycin therapy should engage in regular consultations with their healthcare provider to evaluate their treatment plan and any emerging symptoms. Adjustments to the regimen may improve outcomes and minimize adverse effects.
Patient Adherence and Treatment Outcome
Adherence to prescribed azithromycin therapy significantly influences treatment outcomes. Maintaining consistency with the medication schedule enhances the likelihood of positive results. Patients should take the full course of treatment as directed, even if symptoms improve before completing the regimen.
Research highlights that adherence rates can vary, with many patients experiencing barriers such as side effects, misunderstanding dosage schedules, or forgetting doses. Addressing these challenges can lead to improved outcomes. Clear communication about medication instructions, potential side effects, and the importance of completing the course fosters better adherence.
Once patients understand the impact of incomplete treatment–such as the risk of developing resistance–they often commit more fully to the regimen. Regular follow-ups with healthcare providers can reinforce the need for adherence and allow for adjustments in therapy if side effects occur.
Using reminder systems, such as alarms or mobile apps, can also improve adherence by helping patients remember their dosing schedule. Educational materials that detail the benefits of full treatment compliance and the risks associated with non-adherence provide valuable reinforcement.
Data shows that patients who adhere to treatment protocols have lower rates of recurrence and complications from infections being treated with azithromycin. Promoting a supportive environment, where patients feel comfortable discussing their struggles with adherence, enhances overall treatment success.
Future Directions in Azithromycin Therapy Research
Research should focus on optimizing azithromycin dosing strategies to enhance therapeutic outcomes while minimizing resistance development. Investigators are encouraged to explore shorter treatment regimens in specific infections, such as community-acquired pneumonia and sinusitis, assessing their efficacy and safety compared to standard durations.
Future studies can also examine the role of azithromycin in combination therapies. By investigating its synergistic effects with other antibiotics, particularly in multidrug-resistant infections, researchers could improve clinical outcomes and broaden its application in complex cases.
Investigating the pharmacokinetics of azithromycin in various populations will provide insights into personalized medicine approaches. Identifying factors like age, weight, and comorbidities can lead to tailored dosing recommendations, optimizing treatment for diverse patient groups.
Research into azithromycin’s anti-inflammatory properties may reveal new applications beyond its antimicrobial effects. Exploring its role in chronic inflammatory conditions could open avenues for novel therapies, contributing to a better understanding of its mechanisms outside traditional uses.
Lastly, ongoing surveillance of resistance patterns is crucial. Systematic collection of resistance data will inform treatment guidelines and support public health initiatives aimed at combating antibiotic resistance. By aligning research with clinical needs, azithromycin can maintain its relevance in future therapeutic protocols.