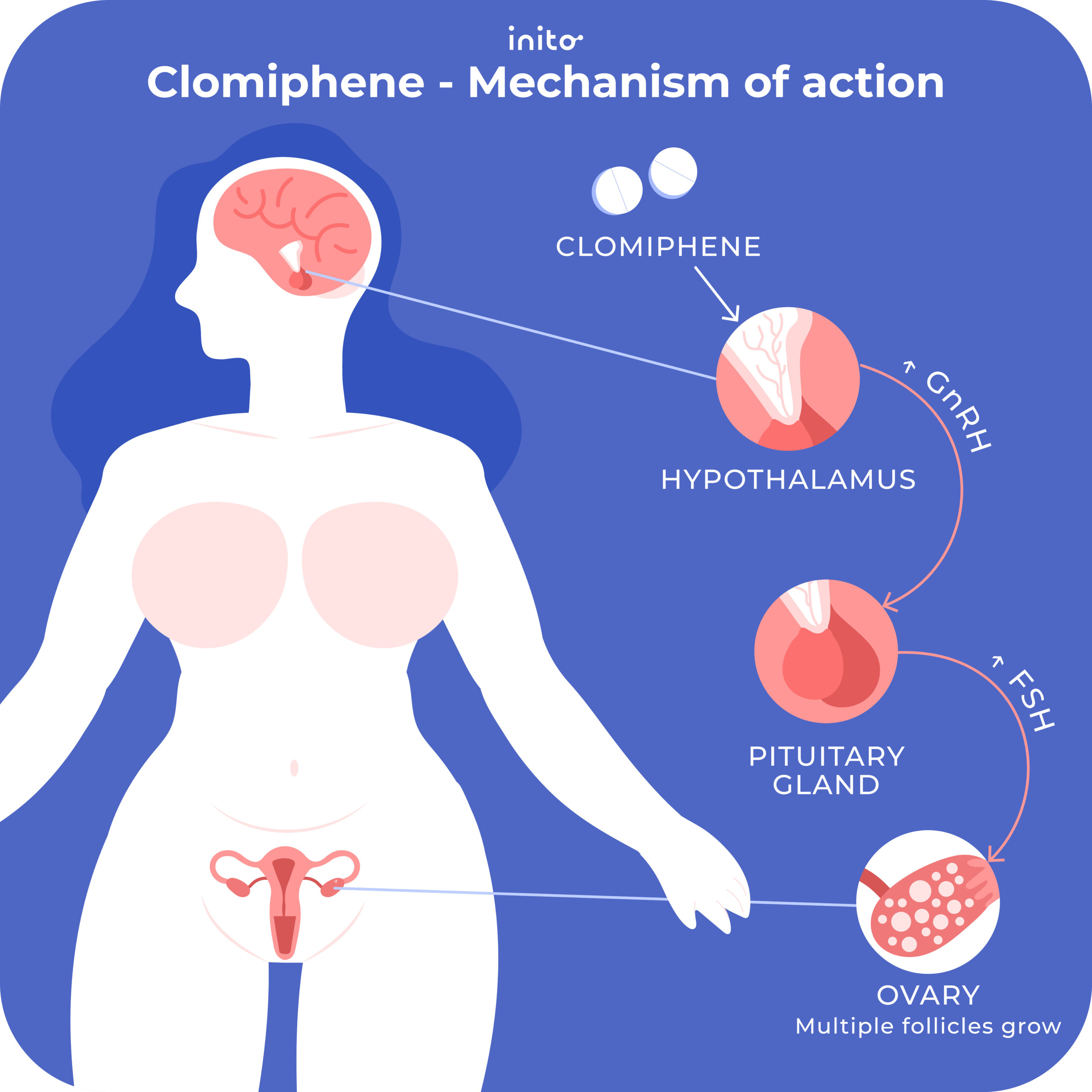
Clomid, also known as clomiphene citrate, primarily targets the hormones responsible for ovulation. It effectively stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which play critical roles in promoting the growth and release of ova from the ovaries.
This medication is often prescribed to women facing challenges with fertility due to ovulatory disorders. By prompting the pituitary gland to produce more FSH and LH, Clomid encourages the ovaries to produce eggs. The result is an increased chance of conception for those struggling to conceive.
Understanding the hormonal impact of Clomid offers a clearer picture of its function. When taken as directed, it can lead to a more regular ovulatory cycle, which is essential for women aiming to enhance their chances of getting pregnant. The role of Clomid in fertility treatment has proven invaluable for many couples along their path to parenthood.
- What Hormone is Clomid
- Overview of Clomid: Mechanism of Action
- Stimulating Ovulation
- Monitoring Response
- Role of Estrogen in Clomid’s Function
- Clomid and the Hypothalamic-Pituitary-Gonadal Axis
- Effects of Clomid on Follicle-Stimulating Hormone (FSH) Levels
- Mechanism of Action
- Clinical Implications
- Common Indications for Clomid Usage
- Possible Side Effects and Hormonal Impacts of Clomid
- Common Side Effects
- Hormonal Impacts
What Hormone is Clomid
Clomid, or clomiphene citrate, primarily influences estrogen receptors in the hypothalamus. This action stimulates the pituitary gland to increase the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Elevated levels of FSH and LH promote ovarian stimulation, encouraging follicle development and ovulation.
This medication is widely used in treating female infertility, particularly in cases of anovulation or oligoovulation. By enhancing the body’s natural hormonal signals, Clomid can lead to successful ovulation cycles.
Additionally, Clomid can have a role in treating male infertility through its impact on testosterone levels by the stimulation of the pituitary gland, although this use is less common. Regular monitoring by a healthcare provider during Clomid therapy is advisable to optimize dosing and assess response.
Consult with a healthcare professional to discuss the benefits and risks associated with Clomid, as well as alternative treatments tailored to individual health needs.
Overview of Clomid: Mechanism of Action
Clomid, known scientifically as clomiphene citrate, mimics estrogen in the body. Its primary role lies in stimulating ovulation in women experiencing infertility. Clomid binds to estrogen receptors in the hypothalamus, disrupting the negative feedback loop that typically inhibits gonadotropin-releasing hormone (GnRH) production. This leads to an increase in GnRH, triggering the pituitary gland to produce more follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Stimulating Ovulation
By elevating FSH and LH levels, Clomid promotes ovarian follicle development and ovulation. Women taking Clomid often experience a rise in the number of follicles, enhancing the chances of conception. It is typically prescribed for a 5-day cycle, starting on the second to fifth day of the menstrual cycle, which maximizes its effectiveness in achieving ovulation.
Monitoring Response
Close monitoring through ultrasound and hormone level assessments is recommended to evaluate the response to Clomid. Adjustments to dosage may be necessary based on the ovarian response. Understanding these mechanics allows healthcare providers to tailor treatment plans, thus improving fertility outcomes for those trying to conceive.
Role of Estrogen in Clomid’s Function
Estrogen plays a key role in the mechanism of Clomid (clomiphene citrate), a medication commonly used to treat infertility in women. By blocking estrogen receptors in the hypothalamus, Clomid creates a perception of low estrogen levels in the body. This triggers the release of gonadotropin-releasing hormone (GnRH), stimulating the pituitary gland to increase the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Higher levels of FSH promote ovarian follicle development, leading to the maturation of eggs. Consequently, this mimetic effect of low estrogen encourages the ovaries to produce more follicles than usual, enhancing the chances of ovulation. Estrogen’s role in this feedback loop is crucial; it shows how this hormone both regulates and responds to reproductive signaling.
As the follicles mature, they produce increasing amounts of estrogen. This rise in estrogen is necessary to maintain a healthy ovarian environment and prepares the uterus for potential implantation. Clinicians monitor estrogen levels during Clomid cycles to assess treatment effectiveness and adjust dosages if necessary.
In summary, estrogen is integral to Clomid’s function by facilitating hormonal communication that promotes follicle development and ovulation. Understanding this relationship can help patients and healthcare providers optimize treatment strategies for infertility.
Clomid and the Hypothalamic-Pituitary-Gonadal Axis
Clomid, or clomiphene citrate, plays a pivotal role in regulating the hypothalamic-pituitary-gonadal (HPG) axis. This medication primarily stimulates the release of gonadotropins, which are crucial for reproductive function.
By blocking estrogen receptors in the hypothalamus, Clomid effectively increases the secretion of gonadotropin-releasing hormone (GnRH). This increase leads to enhanced stimulation of the pituitary gland, resulting in higher levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). The elevation of these hormones initiates ovarian stimulation and promotes follicular development.
It is important for users of Clomid to monitor key hormone levels. The table below summarizes the hormonal changes typically observed when using Clomid:
| Hormone | Before Clomid | During Clomid Treatment |
|---|---|---|
| GnRH | Low | Increased |
| LH | Low | Increased |
| FSH | Low | Increased |
| Estrogen | Normal | Variable |
Understanding these interactions helps in optimizing treatment protocols for individuals experiencing infertility issues. Regular hormone level checks can guide healthcare providers in adjusting Clomid dosage for maximum effectiveness. Proper management of the HPG axis can lead to successful ovulation and pregnancy in many cases.
Effects of Clomid on Follicle-Stimulating Hormone (FSH) Levels
Clomid, or clomiphene citrate, influences levels of Follicle-Stimulating Hormone (FSH) in a notable way. It acts as a selective estrogen receptor modulator (SERM), which can lead to an increase in FSH levels in the body.
Mechanism of Action
Clomid binds to estrogen receptors in the hypothalamus. This binding blocks the effects of circulating estrogen, tricking the body into believing that estrogen levels are low. Consequently, the hypothalamus stimulates the pituitary gland to release more FSH and Luteinizing Hormone (LH).
Clinical Implications
Elevated FSH levels prompt the ovaries to stimulate follicle development, which is crucial for ovulation. Specifically:
- Pregnancy rates improve as ovarian response enhances.
- In patients with certain types of infertility, higher FSH levels may correlate with increased chances of successful ovulation.
- Regular monitoring of FSH levels can help in adjusting Clomid dosage for optimal results.
Patients undergoing Clomid therapy should consult with their healthcare providers for individualized monitoring and dosage adjustments based on their hormonal profile. Understanding these dynamics can significantly influence treatment outcomes.
Common Indications for Clomid Usage
Clomid, or clomiphene citrate, is primarily prescribed for treating ovulatory dysfunction in women trying to conceive. It stimulates the release of hormones necessary for ovulation, making it a go-to option for those facing infertility issues due to irregular menstrual cycles.
This medication is particularly effective for women diagnosed with polycystic ovary syndrome (PCOS), helping to induce ovulation when anovulation is a concern. Clomid increases the chances of pregnancy by encouraging follicle development in the ovaries.
Another indication for Clomid use is unexplained infertility. If standard fertility tests show no clear reasons for conception challenges, Clomid may be recommended. It can help enhance ovarian function, leading to potential ovulation and improved chances of pregnancy.
Clomid is also indicated for male patients with certain types of hypogonadism. By influencing hormonal balance, it may improve sperm production and overall fertility in men.
Monitoring is crucial while using Clomid. Regular ultrasound assessments can track ovarian response and follicle growth, ensuring the appropriate dosage while minimizing risks such as ovarian hyperstimulation syndrome.
In summary, Clomid serves as an effective treatment for ovulatory dysfunction, PCOS-related infertility, unexplained infertility, and select cases of male infertility, enhancing fertility prospects for those affected. Consult with a healthcare provider to evaluate suitability and tailor the approach to individual needs.
Possible Side Effects and Hormonal Impacts of Clomid
Clomid, or clomiphene citrate, may cause various side effects and hormonal changes. Awareness of these effects helps in managing expectations during treatment.
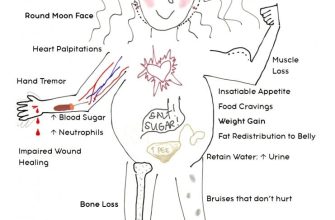
Common Side Effects
- Hot flashes: Many users experience sudden feelings of warmth, typically in the upper body.
- Abdominal discomfort: Some report bloating or mild cramping.
- Headaches: Headaches can occur due to hormonal fluctuations.
- Mood swings: Hormone changes may lead to emotional ups and downs.
- Nausea: Some individuals feel queasy, especially at the beginning of treatment.
Hormonal Impacts
Clomid acts as a selective estrogen receptor modulator, primarily affecting estrogen levels:
- Ovarian response: Stimulation can lead to multiple follicle development.
- Endometrial thickness: Clomid may affect the uterine lining, influencing implantation chances.
- Luteal phase insufficiency: Some women may experience reduced progesterone levels, impacting fertility.
Maintaining communication with a healthcare provider is important. Report any severe or persistent side effects and discuss potential strategies to alleviate discomfort. Regular monitoring ensures a balanced approach to therapy.