Glipizide is a medication primarily used to manage type 2 diabetes. It works by stimulating the pancreas to release more insulin, which helps lower blood sugar levels. If you’re looking for effective ways to control your diabetes, glipizide can be a valuable addition to your treatment plan.
This medication specifically targets blood glucose control by enhancing the body’s response to insulin. When taken before meals, glipizide can significantly reduce post-meal blood sugar spikes, making it a reliable choice for managing daily glucose levels. Regular monitoring of your blood sugar levels while on glipizide is crucial to ensure its effectiveness and adjust dosages as needed.
It’s important to pair glipizide with a balanced diet and regular physical activity. These lifestyle changes complement the medication’s action, providing better overall control of your diabetes. If you experience any side effects, such as low blood sugar, consult your healthcare provider to discuss possible adjustments to your treatment regimen.
In summary, glipizide serves as a key player in diabetes management by enhancing insulin release and lowering blood sugar levels. By following medical advice and maintaining a healthy lifestyle, you can maximize the benefits of glipizide in your diabetes care plan.
- What Does Glipizide Do?
- How It Works
- Usage Guidelines
- Mechanism of Action of Glipizide
- Indications for Glipizide Use
- Dosage Guidelines for Glipizide
- Adjusting Dosage
- Administration Tips
- Common Side Effects of Glipizide
- Drug Interactions with Glipizide
- Common Drug Interactions
- Other Considerations
- Monitoring Blood Sugar Levels while Taking Glipizide
What Does Glipizide Do?
Glipizide helps lower blood sugar levels in individuals with type 2 diabetes. It achieves this by stimulating the pancreas to produce more insulin, allowing the body to utilize glucose effectively. This medication specifically targets glucose regulation following meals, which is crucial for managing postprandial blood sugar spikes.
How It Works
The action of glipizide occurs primarily in the pancreas. By binding to specific receptors on pancreatic beta cells, it enhances insulin secretion. This process often leads to a reduction in blood sugar levels after eating. Additionally, glipizide may decrease glucose production in the liver, contributing to overall glucose control.
Usage Guidelines
Typically, glipizide is taken orally, with the timing based on meals to optimize its impact. Regular monitoring of blood sugar levels is advisable to ensure the medication is working effectively. It is important to follow healthcare provider recommendations regarding dosage to avoid hypoglycemia, a potential side effect of excessive insulin stimulation.
Mechanism of Action of Glipizide
Glipizide primarily stimulates insulin secretion from the pancreas. It targets the beta cells in the islets of Langerhans, enhancing their ability to release insulin in response to glucose levels in the blood.
This medication binds to specific sites on the sulfonylurea receptor (SUR1), a component of the ATP-sensitive potassium channels located on the beta cell membrane. By closing these potassium channels, glipizide results in depolarization of the cell membrane, which leads to an influx of calcium ions (Ca2+). This increase in intracellular calcium levels triggers insulin secretion.
In addition to enhancing insulin release, glipizide contributes to improved tissue sensitivity to insulin, which aids in better glucose utilization by muscle and fat tissues. It also reduces hepatic glucose production, further helping to decrease overall blood sugar levels.
- Stimulates insulin release from pancreatic beta cells.
- Binds to sulfonylurea receptor, closing ATP-sensitive potassium channels.
- Increases intracellular calcium, promoting insulin secretion.
- Improves tissue sensitivity to insulin.
- Reduces hepatic glucose output.
Patients taking glipizide should monitor their blood glucose levels regularly and report significant changes to their healthcare provider. This will help ensure optimal management of diabetes and prevent potential hypoglycemic episodes.
Indications for Glipizide Use
Glipizide is primarily prescribed for managing type 2 diabetes mellitus. It enhances insulin secretion from the pancreas, which lowers blood sugar levels effectively. Several specific indications for its use include:
- Type 2 Diabetes Management: Glipizide is suitable for patients whose blood sugar levels remain uncontrolled with diet and exercise alone.
- Adjunct Therapy: It can be used alongside other antidiabetic agents, such as metformin, to achieve better glycemic control.
- Postprandial Glucose Control: Glipizide helps reduce blood sugar spikes that occur after meals.
- Insulin Sensitivity Improvement: It may enhance the body’s sensitivity to insulin over time, further contributing to glucose regulation.
Healthcare providers often consider Glipizide for patients who:
- Experience symptoms of hyperglycemia.
- Require oral medication due to contraindications or intolerance to insulin therapy.
- Demonstrate a need for personalized treatment strategies focusing on blood sugar control.
Monitoring blood glucose levels regularly is essential for patients on Glipizide to ensure the medication is achieving desired outcomes and to adjust dosages as necessary.
Always consult a healthcare professional to discuss any potential side effects and to tailor the treatment plan to individual health needs.
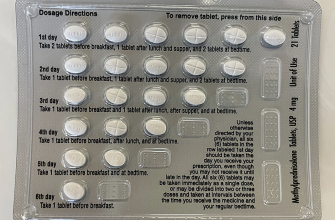
Dosage Guidelines for Glipizide
Initiate treatment with glipizide at a starting dose of 5 mg once daily, taken before breakfast. Depending on individual blood glucose levels, adjust the dosage in increments of 2.5 mg or 5 mg. The maximum recommended dose does not exceed 20 mg daily.
Adjusting Dosage
Monitor blood glucose levels regularly to effectively guide dosage adjustments. If control remains insufficient, consider increasing the dose every few weeks. Conversely, if hypoglycemia occurs, reduce the dose promptly or consider switching to a different medication. For patients with reduced renal function, initiate at lower doses and adjust cautiously.
Administration Tips
Take glipizide with food to enhance absorption and minimize the risk of gastrointestinal discomfort. Swallow the tablet whole; do not crush or chew. Consistency in the timing of doses helps maintain stable glucose levels throughout the day. Always follow your healthcare provider’s specific instructions regarding use and adjustments.
Common Side Effects of Glipizide
Taking glipizide can lead to specific side effects. Patients should monitor their reactions closely. Hypoglycemia is one of the most common issues; watch for symptoms like dizziness, sweating, and confusion. Regularly check blood sugar levels to prevent this condition.
Gastrointestinal disturbances may occur. Many report nausea, vomiting, or diarrhea. Eating smaller, more frequent meals can help alleviate these symptoms. If they persist, consult a healthcare provider.
Weight gain might also arise. To manage weight, maintain a balanced diet and incorporate physical activity into your routine. Discuss any concerns with a healthcare provider to explore alternative treatments if necessary.
Some individuals experience allergic reactions. Look for signs such as rash, itching, or swelling. If these symptoms develop, seek medical attention right away.
Lastly, fatigue or a general feeling of tiredness can impact daily life. Ensure adequate hydration and rest. If fatigue continues, it’s essential to speak with a healthcare professional.
Staying informed about potential side effects promotes better management of your health while on glipizide.
Drug Interactions with Glipizide
Glipizide may interact with various medications, influencing blood sugar levels or increasing the risk of side effects. Be proactive about reviewing any concurrent medications with your healthcare provider.
Common Drug Interactions
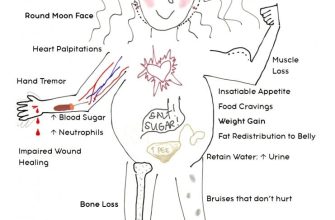
Some medications can reduce glipizide’s effectiveness. Beta-blockers often mask hypoglycemia symptoms, making it harder to recognize low blood sugar. Corticosteroids may raise blood sugar levels, counteracting glipizide’s effects. Thiazide diuretics can also raise glucose levels, leading to inadequate control of diabetes.
Other Considerations
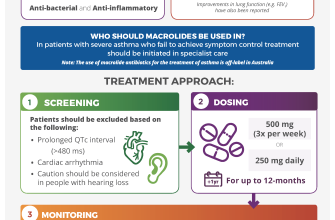
Alcohol consumption can significantly impact blood sugar levels. It’s advisable to limit alcohol intake while taking glipizide. Assess macrolide antibiotics, like erythromycin, since they may enhance glipizide’s effect. Always inform your doctor about all medications, supplements, and herbal products you use to ensure safe and effective treatment.
Monitoring Blood Sugar Levels while Taking Glipizide
Regularly monitor your blood sugar levels to ensure that glipizide is managing your diabetes effectively. Check your levels at various times throughout the day, particularly before meals and at bedtime, to understand how glipizide impacts your blood sugar.
Consider the following recommended schedule for testing:
| Time of Day | Recommended Action |
|---|---|
| Before Breakfast | Test to assess fasting levels. |
| Before Lunch | Monitor to adjust food intake. |
| Before Dinner | Check levels to avoid hypoglycemia. |
| Bedtime | Ensure safe levels overnight. |
Always document your readings. Share this data with your healthcare provider during appointments to adjust your treatment plan as necessary. Be alert for signs of low blood sugar, such as dizziness, shaking, or sweating, and know how to respond. A quick source of glucose, like glucose tablets or juice, should be readily available.
Follow your healthcare provider’s instructions regarding diet and exercise, as these factors significantly impact blood sugar control. Consistent monitoring and communication with your healthcare team will enhance your management of diabetes while taking glipizide.