Risperdal, also known as risperidone, is often prescribed for managing behavioral symptoms in elderly patients with dementia. Research indicates that this atypical antipsychotic can effectively reduce symptoms such as aggression, agitation, and psychosis. However, it’s essential to weigh potential benefits against risks, particularly the heightened sensitivity of this demographic to side effects.
For optimal results, healthcare providers should initiate treatment at the lowest possible dose, adjusting as necessary while closely monitoring for adverse reactions. Start with a dose of 0.5 mg per day, gradually increasing to a maximum of 1-2 mg per day based on patient tolerance and response. Regular follow-ups are crucial to assess the patient’s mental state, physical health, and overall quality of life.
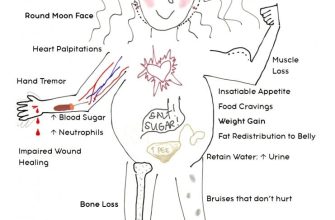
While Risperdal can provide significant benefits, awareness of potential risks, including metabolic syndrome and extrapyramidal symptoms, is critical. Monitor patients for weight gain, blood glucose levels, and any motor disturbances. This proactive approach ensures the safety and well-being of elderly individuals navigating the complexities of dementia care.
- Risperdal in Elderly with Dementia
- Dosage and Administration
- Risks and Benefits
- Understanding Dementia and Its Behavioral Symptoms
- Risperdal: Mechanism of Action in Treating Behavioral Symptoms
- Additional Mechanisms
- Clinical Guidelines for Prescribing Risperdal in Dementia Patients
- Assess Risks and Benefits
- Regular Monitoring
- Benefits and Limitations of Risperdal for the Elderly
- Monitoring and Managing Side Effects of Risperdal
- Case Studies: Efficacy of Risperdal in Elderly with Dementia
- Alternatives to Risperdal for Behavioral Management in Dementia
- Non-Pharmacological Approaches
- Alternative Medications
Risperdal in Elderly with Dementia
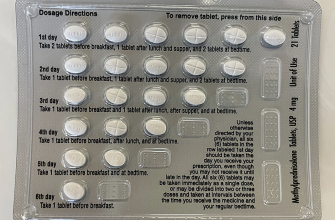
Prescribing Risperdal (risperidone) for elderly patients with dementia requires careful consideration of dosage and potential side effects. Start with the lowest possible dose, typically 0.5 mg daily, and monitor for efficacy and tolerability.
Dosage and Administration
Gradually titrate the dose based on the patient’s response, with the maximum recommended dose not exceeding 1-2 mg daily. Regular follow-up visits assess behavioral symptoms and overall health, adjusting the dose as needed. Pay attention to the signs of sedation, weight gain, and extrapyramidal symptoms.
Risks and Benefits
Evaluating the risks is crucial. Elderly patients have a higher sensitivity to medications, increasing the likelihood of adverse effects. Monitor for potential cardiovascular issues, metabolic syndrome, and any signs of infection. Weigh the benefits of improved agitation and psychosis against these risks. Emphasize non-pharmacological approaches as a complementary strategy for managing symptoms.
Risperdal can be beneficial, but a thorough assessment of each patient is vital. Regularly review treatment plans and involve caregivers in monitoring changes in behavior to ensure the best outcomes.
Understanding Dementia and Its Behavioral Symptoms
Dementia significantly impacts cognitive functions, resulting in a variety of behavioral symptoms that can be distressing for both patients and caregivers. Recognizing these symptoms early allows for timely interventions.
Common behavioral symptoms include:
- Aggression and Agitation: Patients may exhibit irritability or respond explosively to stimuli. Identifying triggers in the environment can help manage these reactions.
- Withdrawal: Social isolation often occurs. Encouraging gentle social interactions can help maintain connections and reduce feelings of loneliness.
- Loss of Interest: Individuals may lose enthusiasm for activities they once enjoyed. Introducing new, simple activities can rekindle interest.
- Anxiety and Depression: Feelings of fear or sadness are common. Regular routines and familiarity can provide comfort and stability.
Effective communication strategies enhance interactions:
- Simplify language. Use short, clear sentences.
- Maintain eye contact to convey attention and understanding.
- Employ non-verbal cues, such as gestures or facial expressions, to support verbal messages.
A proactive approach to managing these symptoms is crucial. Establishing a predictable routine can mitigate confusion and anxiety. Observing behavior patterns helps caregivers anticipate needs and react appropriately.
Involvement in meaningful activities tailored to individual preferences offers therapeutic benefits. Activities should promote engagement without overwhelming the individual.
Training for caregivers enhances their understanding of dementia. Knowledge about the disease equips them to handle challenging situations calmly and compassionately.
Lastly, consider consulting health professionals when behavioral symptoms escalate. Medication, like Risperdal, may be appropriate in specific cases but should be evaluated carefully due to potential side effects in elderly patients.
Risperdal: Mechanism of Action in Treating Behavioral Symptoms
Risperdal acts primarily as an antagonist at dopamine D2 and serotonin 5-HT2A receptors. This dual mechanism effectively balances neurotransmitter activity, targeting the behavioral symptoms associated with dementia in elderly patients.
The inhibition of dopamine D2 receptors reduces psychotic manifestations, such as agitation and aggression. By blocking these receptors, Risperdal mitigates overactivity in dopaminergic pathways, which often contributes to behavioral disturbances.
Simultaneously, the antagonism at serotonin 5-HT2A receptors plays a critical role in enhancing mood and decreasing anxiety levels. This interaction fosters a calming effect, improving overall social engagement and interaction, which is significant for dementia patients.
Additional Mechanisms
Risperdal also influences other neurotransmitter systems such as norepinephrine and histamine, enhancing its efficacy in managing behavioral symptoms. The medication’s ability to modulate these pathways promotes a more balanced emotional state in patients.
| Receptor Type | Effect |
|---|---|
| Dopamine D2 | Reduces psychotic symptoms |
| Serotonin 5-HT2A | Improves mood and decreases anxiety |
| Norepinephrine | Enhances mood stability |
| Histamine | Reduces agitation and restlessness |
In summary, Risperdal’s multifaceted approach effectively addresses behavioral symptoms in elderly patients with dementia, contributing to improved quality of life and better management of their condition.
Clinical Guidelines for Prescribing Risperdal in Dementia Patients
Begin treatment with the lowest effective dose of Risperdal, typically starting at 0.25 mg to 0.5 mg daily. Assess the patient’s overall health, comorbidities, and existing medications before initiating therapy. Monitor for any adverse effects, especially in elderly patients. Adjust the dosage gradually based on clinical response and tolerability, with a maximum daily dose not exceeding 1.0 mg to 2.0 mg.
Assess Risks and Benefits
Evaluate the patient’s symptoms, the severity of dementia, and overall prognosis. Consider non-pharmacological interventions first, such as behavioral therapies. If medication is necessary, weigh the potential benefits of Risperdal for agitation and aggression against risks, including sedation and potential cardiovascular issues.
Regular Monitoring
Conduct regular evaluations to monitor for response to treatment and side effects. Schedule follow-up visits at least every month for the first three months of therapy, then every 3-6 months as needed. Pay close attention to signs of extrapyramidal symptoms, metabolic syndrome, and changes in mental status. Adjust treatment based on findings during these evaluations, ensuring the patient’s quality of life remains a priority.
Benefits and Limitations of Risperdal for the Elderly
Risperdal can alleviate behavioral symptoms in elderly patients with dementia, effectively reducing agitation, irritability, and aggression. Clinical studies indicate a significant improvement in these areas, promoting a calmer environment for both patients and caregivers.
One notable advantage is its ability to enhance quality of life. Many patients experience better social interaction and improved engagement in daily activities. This medication can facilitate a more stable emotional state, allowing caregivers to implement non-pharmacological interventions more successfully.
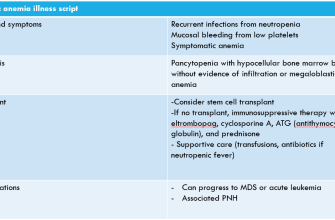
On the downside, the use of Risperdal in older adults carries risks. Common side effects include sedation and increased fall risk, which can lead to serious injuries. Additionally, the potential for metabolic changes, such as weight gain and diabetes, warrants careful monitoring.
Long-term use may lead to extrapyramidal symptoms or tardive dyskinesia, raising concerns regarding prolonged treatment duration. Regular assessments of the patient’s response and side effects are crucial to managing these risks effectively.
Balancing the benefits against possible adverse effects is essential. A low starting dose is recommended, with gradual adjustments based on the patient’s response and tolerance. Collaboration with healthcare providers ensures a tailored approach, improving outcomes while minimizing risks.
Monitoring and Managing Side Effects of Risperdal
Regularly monitor elderly patients on Risperdal for common side effects. Pay close attention to the following:
- Extrapyramidal Symptoms (EPS): Look for signs like tremors, rigidity, and bradykinesia. Assess motor function frequently, especially during dosage adjustments.
- Weight Gain: Track weight monthly. Implement dietary modifications and encourage physical activity to mitigate this effect.
- Metabolic Changes: Check glucose and lipid levels at baseline, and then at least annually. Maintain awareness of diabetes-related symptoms, such as increased thirst or urination.
- Cardiovascular Issues: Monitor blood pressure and heart rate regularly. Be alert for signs of orthostatic hypotension, especially during the initial phase of treatment.
- sedation: Note changes in alertness or excessive drowsiness. Adjust dosages accordingly, ensuring safety during daily activities.
Provide education to caregivers about these potential side effects. Encourage them to report any concerning symptoms immediately. Offer reassurance and support, ensuring they feel empowered to manage the patient’s care.
Regular follow-up appointments allow for timely assessment of the patient’s response to treatment. These visits should include:
- Review of any reported side effects or concerns.
- Adjustment of medication dosages based on tolerance and effectiveness.
- Discussion regarding the overall management of dementia symptoms and the role of Risperdal.
Utilize standardized rating scales to objectively measure changes in behavior and side effects. This aids in documenting the patient’s progress and ensuring appropriate adjustments are made swiftly.
In summary, proactive monitoring and management of side effects are vital in enhancing the overall quality of life for elderly patients taking Risperdal.
Case Studies: Efficacy of Risperdal in Elderly with Dementia
Risperdal shows promise in managing psychiatric symptoms in elderly patients with dementia. A case study involving a 78-year-old female patient with moderate Alzheimer’s demonstrated a significant decrease in agitation and aggression levels after initiating treatment with Risperdal at a low dose of 0.5 mg daily. Caregivers reported improved daily functioning and a reduction in the frequency of disruptive behaviors within four weeks of treatment.
In another instance, an 82-year-old male with vascular dementia exhibited severe paranoia and hostility. After a careful assessment, the treatment plan included Risperdal, starting at 1 mg per day. Following two months on the medication, the patient’s anxiety levels diminished, allowing for better social interactions and an enhanced quality of life as noted by family members and staff.
Additionally, a clinical trial highlighting Risperdal’s impact revealed that 60% of participants experienced a significant reduction in neuropsychiatric symptoms. The most pronounced effects were seen in patients with mixed dementia, where a dosage titration approach helped achieve optimal results while minimizing side effects.
Monitoring for side effects is critical. In cases where patients experienced sedation or extrapyramidal symptoms, dose adjustments led to improved tolerability. Regular follow-ups ensured that each individual’s response guided ongoing treatment plans.
These case studies illustrate the potential benefits of Risperdal when used judiciously in the management of behavioral symptoms associated with dementia in elderly patients. Individualized treatment strategies contribute to improved outcomes and better overall care. Collaboration among healthcare providers, caregivers, and family members remains vital to successful interventions.
Alternatives to Risperdal for Behavioral Management in Dementia
Choosing alternatives to Risperdal for managing behavioral symptoms in dementia can enhance patient care. A combination of non-pharmacological methods and alternative medications offers promising results.
Non-Pharmacological Approaches
Therapeutic Activities: Engaging patients in meaningful activities tailored to their interests can reduce agitation. Art therapy, music therapy, and reminiscence therapy have shown positive effects in managing anxiety and aggression.
Environmental Modifications: Adjusting the living environment to minimize confusion can create a calming atmosphere. Utilizing familiar objects, reducing noise, and ensuring adequate lighting can significantly enhance comfort levels.
Alternative Medications
Sertraline: This selective serotonin reuptake inhibitor has been effective in reducing anxiety and depressive symptoms in dementia patients. Its favorable side effects profile makes it a suitable choice.
Quetiapine: Often used as an alternative, this atypical antipsychotic manages agitation and psychotic symptoms with a lower risk of extrapyramidal symptoms compared to traditional antipsychotics.
Buspirone: An anti-anxiety medication that offers a gentle approach to managing agitation, particularly in patients with anxiety symptoms, and is well-tolerated.
Using these alternatives can often lead to improved quality of life for individuals with dementia. Caregivers should assess each patient’s specific needs and closely monitor any implemented changes.