Consider a prednisone burst therapy regimen when asthma symptoms escalate and conventional treatments fall short. This approach typically involves administering a high dose of prednisone over a short period, allowing for rapid control of inflammation and relief from wheezing and shortness of breath. Studies show that a 5 to 7-day course of prednisone, starting at 40 to 60 mg per day for adults, can significantly improve lung function and overall well-being.
During a burst, monitor your symptoms closely and maintain open communication with your healthcare provider. Dosage adjustments may be necessary based on individual responses and side effects. Introduce this treatment after assessing your asthma action plan and ensuring that any rescue medications are readily available. Using a peak flow meter can also help track your lung function and determine the effectiveness of the therapy.
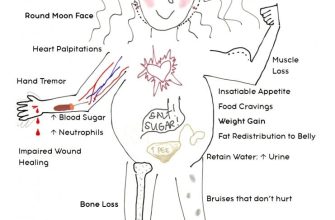
Don’t ignore potential side effects, such as mood changes, increased appetite, or difficulty sleeping. While these are common, discuss any concerning symptoms with your doctor to manage them effectively. Combining prednisone burst therapy with your regular asthma management plan can lead to improved daily functioning and a reduction in severe exacerbations.
- Prednisone Burst Therapy for Asthma
- Understanding Prednisone and Its Role in Asthma Management
- Indications for Prescribing Prednisone Burst Therapy
- Typical Dosage and Administration Guidelines for Asthma Patients
- Dosage Adjustment and Monitoring
- Administration Tips
- Potential Side Effects and Risks of Prednisone Therapy
- Monitoring and Follow-Up Care During Prednisone Treatment
- Medication Adherence and Education
- Monitoring Comorbidities
Prednisone Burst Therapy for Asthma
Administer prednisone for a short course during asthma exacerbations. This therapy typically consists of a high dose for a brief period, usually ranging from five to seven days. Prednisone helps reduce inflammation and opens airways, providing quick relief for patients experiencing worsening asthma symptoms.
Start with a dose based on the individual’s weight and severity of symptoms. For adults, a common starting dose is between 40 to 60 mg per day. For children, dosing is adjusted to around 1 mg per kilogram of body weight, not exceeding 60 mg daily.
Monitor patients closely during the treatment. Check for side effects such as increased appetite, mood changes, and sleep disturbances. These typically resolve after discontinuation of the medication. Advise patients to avoid stopping prednisone abruptly; tapering off is critical to prevent adrenal insufficiency.
Incorporate this therapy with a comprehensive asthma management plan. Encourage regular medication adherence for preventive inhalers and continued monitoring of asthma triggers. Follow up with patients to assess their response to the burst therapy and make any necessary adjustments to their ongoing treatment regimen.
This approach offers rapid improvement in symptoms, helping patients regain control of their asthma promptly. Encourage communication about any concerns or persisting symptoms to ensure optimal care.
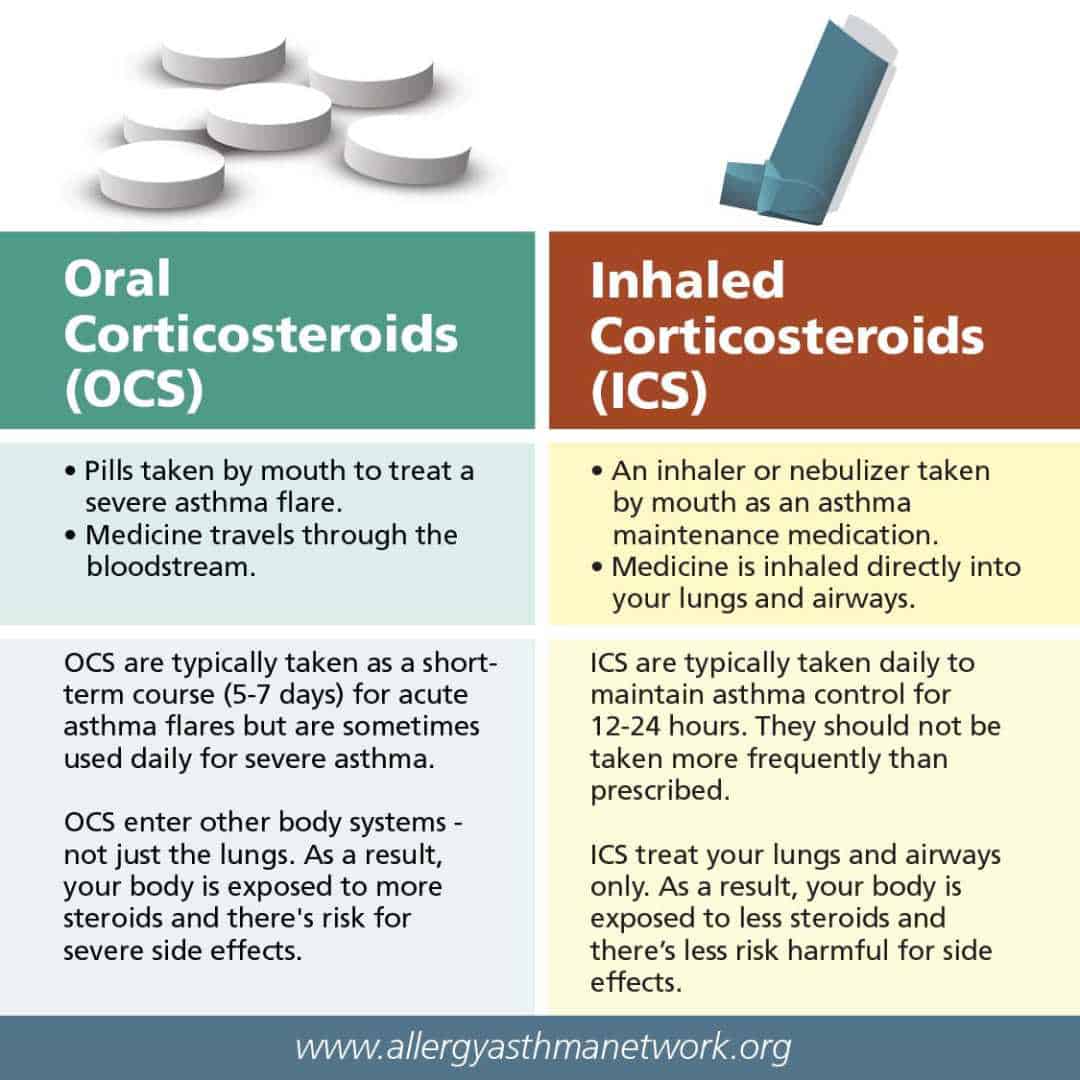
Understanding Prednisone and Its Role in Asthma Management
Prednisone serves as a steroid medication that helps reduce inflammation in the airways. For asthma patients experiencing acute exacerbations, a burst therapy of prednisone can provide rapid relief. Typically, this involves higher doses taken over a short period, often for about 3 to 10 days, depending on the severity of the symptoms.
This therapy targets the underlying inflammation that leads to airway narrowing and reduced airflow. Prednisone dampens immune responses and decreases the production of inflammatory substances in the body, allowing the airways to open up and improve breathing.
For effective use, healthcare providers usually monitor symptoms and adjust dosages based on a patient’s response. It’s crucial to start the therapy at the onset of worsening symptoms to maximize its benefits. Following a prescribed tapering schedule after a burst can help prevent potential withdrawal symptoms and complications.
Patients should be aware of possible side effects, such as increased appetite, mood changes, and fluid retention. Staying in touch with a healthcare provider during and after treatment ensures proper management of these effects and overall asthma control.
Incorporating prednisone burst therapy into an asthma management plan can significantly improve quality of life and reduce the necessity for emergency interventions. Always consult with a healthcare professional to determine the best approach tailored to individual needs.
Indications for Prescribing Prednisone Burst Therapy
Prednisone burst therapy is recommended for patients experiencing severe asthma exacerbations that do not improve with standard bronchodilator treatment. This therapy aims to reduce inflammation and enhance airflow. Indications for prescribing this treatment include:
- Acute Asthma Attacks: Patients with significant respiratory distress or wheezing that is unresponsive to rescue inhalers.
- Frequent Exacerbations: Individuals with multiple exacerbations within a short period, suggesting inadequate control of asthma.
- Severe Symptoms: Symptoms such as persistent cough, chest tightness, or fatigue affecting daily activities.
- History of Hospitalization: Patients with a history of severe asthma-related hospitalizations require close monitoring and potential steroid therapy.
- Marked Decrease in Peak Flow: A significant drop in peak expiratory flow readings compared to baseline measurements.
Before initiating therapy, assess the patient’s history, current medication regimen, and potential contraindications. Monitor for side effects during treatment, and establish a follow-up plan to evaluate the response to therapy and adjust the asthma management strategy accordingly.
Long-term management strategies should be reviewed and tailored after the acute episode resolves to maintain optimal asthma control and minimize future exacerbations.
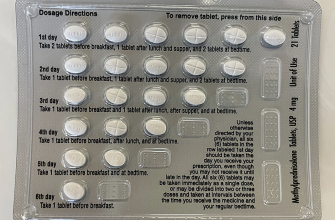
Typical Dosage and Administration Guidelines for Asthma Patients
For asthma patients undergoing prednisone burst therapy, the dosage typically starts at 40-60 mg per day. Healthcare providers often recommend this dosage for 5-7 days during exacerbations. Individual needs may vary, so adjusting the dosage based on the patient’s response to treatment is common practice.
Dosage Adjustment and Monitoring
Monitor the patient’s symptoms closely. If there is insufficient improvement after three days, consider reevaluating the treatment plan or increasing the dosage. Once symptoms stabilize, taper the prednisone dose gradually to avoid rebound effects.
Administration Tips
Administer prednisone orally, preferably with food to minimize gastrointestinal upset. Encourage patients to take their medication consistently at the same time each day. If a dose is missed, instruct them to take it as soon as they remember, unless it’s close to the next scheduled dose.
| Time Period | Dosage | Notes |
|---|---|---|
| Days 1-3 | 40-60 mg daily | Monitor for improvement |
| Days 4-5 | May reduce to 20-40 mg daily | Taper based on response |
| Days 6-7 | Consider tapering further | Complete course if symptoms resolve |
Regular follow-ups with healthcare providers ensure effective management of asthma symptoms and optimal use of prednisone therapy. Encourage patients to report any side effects promptly.
Potential Side Effects and Risks of Prednisone Therapy
Regularly monitor patients on prednisone therapy for potential side effects. Recognizing these can lead to timely interventions and minimize complications.
- Weight Gain: Prednisone can lead to increased appetite and fat distribution, particularly around the abdomen. Encourage patients to maintain a balanced diet and monitor their caloric intake.
- Fluid Retention: Edema may occur due to sodium retention. Recommend limiting salt intake and monitoring weight changes.
- Blood Sugar Levels: Monitor glucose levels, especially in patients with diabetes, as prednisone may elevate blood sugar. Adjust diabetes medications if necessary.
- Bone Health: Long-term use can result in osteoporosis. Advise patients on calcium and vitamin D supplementation and consider bone density scans.
- Gastrointestinal Issues: Prednisone can induce stomach irritation and ulcers. Suggest taking the medication with food and evaluating for signs of gastrointestinal bleeding.
- Mood Changes: Patients may experience mood swings or increased anxiety. Regularly assess mental health and provide resources for psychological support if needed.
- Increased Infection Risk: Immunosuppression may occur, raising susceptibility to infections. Advise patients to practice good hygiene and seek care promptly for signs of infection.
Educate patients on tapering off prednisone to avoid adrenal insufficiency. Discuss the importance of not abruptly discontinuing the medication. Ensure regular follow-up appointments to reassess the need for continued therapy and monitor side effects thoroughly.
Monitoring and Follow-Up Care During Prednisone Treatment
Schedule regular follow-up appointments to monitor the patient’s response to prednisone therapy. During these visits, assess respiratory function through spirometry or peak flow measurement. Track symptoms of asthma, noting any improvements or deterioration. Adjust treatment based on these evaluations.
Observe for potential side effects of prednisone, which may include weight gain, mood changes, sleep disturbances, and increased blood pressure. Encourage patients to report any unusual symptoms immediately. Implement strategies for managing these side effects, such as dietary adjustments and stress management techniques.
Medication Adherence and Education
Ensure patients understand the importance of adhering to their prescribed prednisone regimen. Discuss potential tapering schedules if they are on long-term therapy to prevent withdrawal symptoms. Provide written materials that explain how to recognize exacerbation signs and when to seek help.
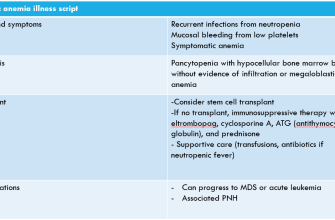
Monitoring Comorbidities
Evaluate the patient’s overall health to identify any comorbid conditions that may affect asthma management. Check for conditions like diabetes, hypertension, or osteoporosis, as prednisone can exacerbate these issues. Collaborate with other healthcare providers to ensure a coordinated approach to the patient’s treatment plan.