Yes, prednisone can suppress cortisol production. This synthetic corticosteroid mimics the effects of hormones your body produces naturally in the adrenal glands. By introducing prednisone into your system, you signal your body to reduce its own cortisol output, leading to lower natural hormone levels.
When using prednisone as a treatment option, especially for conditions like autoimmune disorders or inflammation, it’s essential to monitor cortisol levels closely. Regular blood tests may be necessary to assess how your body responds to the medication and how it affects adrenal function.
Long-term use of prednisone can lead to adrenal insufficiency, a condition where your adrenal glands do not produce adequate amounts of hormones, including cortisol. If you are prescribed prednisone, work closely with your healthcare provider to develop a tapering strategy when discontinuing the medication, ensuring your body has time to resume normal cortisol production.
- Does Prednisone Suppress Cortisol?
- Mechanism of Action: How Prednisone Affects Cortisol Levels
- Effects on Cortisol Production
- Implications for Patients
- Clinical Implications: Effects of Cortisol Suppression in Patients
- Adrenal Insufficiency Risks
- Impact on Metabolism
- Managing Prednisone Use: Strategies to Minimize Cortisol Impact
Does Prednisone Suppress Cortisol?
Yes, prednisone can suppress cortisol production. As a synthetic corticosteroid, prednisone mimics the effects of cortisol in the body. Regular use can lead to a decrease in the body’s natural cortisol levels due to negative feedback on the hypothalamic-pituitary-adrenal (HPA) axis.
During treatment with prednisone, the adrenal glands become less active in producing cortisol, as the body perceives adequate levels due to the medication. This suppression may result in adrenal insufficiency if prednisone is abruptly discontinued, requiring careful tapering to restore natural cortisol production.
Patients on long-term prednisone therapy should monitor for symptoms of adrenal insufficiency, which may include fatigue, weakness, and low blood pressure. Regular consultations with a healthcare provider are important for adjusting medication dosages and preventing complications.
Additionally, blood tests can help assess cortisol levels during and after prednisone use. It is crucial for individuals taking prednisone to follow medical advice closely and report any concerning symptoms to their healthcare team.
Mechanism of Action: How Prednisone Affects Cortisol Levels
Prednisone directly influences cortisol levels through its action as a synthetic glucocorticoid. When administered, it mimics the effects of cortisol, binding to glucocorticoid receptors within the cytoplasm of target cells. This binding triggers a cascade of biological responses, leading to alterations in gene expression that can inhibit the synthesis of endogenous cortisol.
Prednisone modulates the hypothalamic-pituitary-adrenal (HPA) axis by decreasing the release of corticotropin-releasing hormone (CRH) from the hypothalamus and adrenocorticotropic hormone (ACTH) from the pituitary gland. This suppression results in a decrease in adrenal gland stimulation, subsequently lowering the natural production of cortisol.
Effects on Cortisol Production
By reducing ACTH levels, prednisone effectively diminishes the adrenal cortex’s secretion of cortisol. This mechanism can lead to significant alterations in metabolism, immune response, and stress management in the body. Continuous use of prednisone may lead to adrenal suppression, where the adrenal glands reduce their output of cortisol, potentially causing complications if prednisone is abruptly discontinued.
Implications for Patients
Patients on prednisone therapy should be aware of the potential effects on their natural cortisol production. Monitoring cortisol levels may be necessary to avoid adrenal insufficiency when tapering off the medication. Adjusting steroid dosage must be approached cautiously, ensuring that the body can gradually resume normal cortisol production. Regular consultation with healthcare professionals is vital for safe management throughout treatment.
Clinical Implications: Effects of Cortisol Suppression in Patients
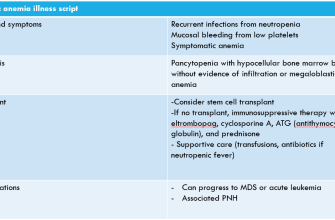
Clinicians should closely monitor patients on prednisone for signs of cortisol suppression. This medication can significantly lower endogenous cortisol production, leading to potential adrenal insufficiency. Patients may experience fatigue, weakness, and an increased risk of infections due to impaired immune function.
Adrenal Insufficiency Risks
Healthcare providers must be vigilant in assessing the risk of adrenal crisis, especially during periods of stress or infection. Patients showing symptoms such as severe fatigue, dizziness, or gastrointestinal distress should be evaluated promptly. Gradual tapering of prednisone is recommended to allow the adrenal glands to resume normal cortisol production.
Impact on Metabolism
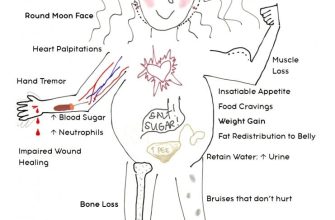
Cortisol suppression can influence metabolism, causing changes in appetite and weight gain. Patients might need nutritional counseling to manage these side effects effectively. Regular weight monitoring and adjustments in diet and exercise can mitigate the impact of these metabolic changes.
Managing Prednisone Use: Strategies to Minimize Cortisol Impact
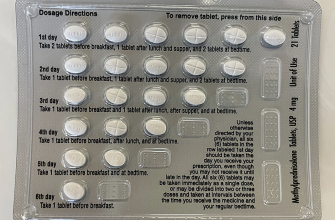
Limit prednisone dosage whenever possible. Work with your healthcare provider to find the lowest effective dose that manages your condition. This helps maintain your natural cortisol levels.
Implement a gradual tapering schedule. If your treatment requires discontinuation, avoid sudden cessation. Instead, slowly reduce the dosage to allow your body to adjust and begin producing cortisol naturally.
Monitor your diet closely. Focus on nutrient-rich foods. Include:
- Fresh fruits and vegetables
- Whole grains
- Lean proteins
- Healthy fats, such as avocados and nuts
This promotes overall health and mitigates some side effects of prednisone.
Integrate regular physical activity into your routine. Engage in moderate exercise, such as walking, swimming, or yoga, to help balance hormone levels. Aim for at least 150 minutes of moderate exercise per week.
Address stress management techniques. Incorporate mindfulness practices like meditation or deep-breathing exercises to decrease stress and help regulate cortisol levels. Regular sleep patterns also play a key role; aim for 7-9 hours of quality sleep each night.
Stay informed about potential side effects. Monitor for signs like weight gain, mood changes, or sleep disturbances. Report these to your healthcare provider for appropriate adjustments to your treatment plan.
Consider supplementation with caution. Some studies suggest that specific vitamins, such as vitamin C and D, may aid adrenal function. Consult your healthcare provider before starting any supplements to ensure they are safe for you.
Finally, maintain open communication with your healthcare team. Discuss any concerns you may have regarding prednisone treatment and cortisol levels. Their guidance is invaluable in achieving the best outcome for your health.