Switching from Plavix to 325 mg of aspirin can be a practical option for managing cardiovascular risks. Research indicates that aspirin serves as an effective antiplatelet agent, lowering the likelihood of blood clots and subsequent heart attacks or strokes. However, the decision should be based on individual health needs, medical history, and specific risk factors.
Aspirin works by inhibiting platelet aggregation, while Plavix, or clopidogrel, activates different pathways to achieve similar outcomes. Some studies suggest that, in certain patients, a low-dose aspirin can provide comparable protection against thrombotic events. It’s imperative to consult with a healthcare provider before making any changes to your medication regimen.
Monitoring is key after switching to aspirin. Regular check-ups can identify any potential side effects like gastrointestinal discomfort or increased bleeding risk. Tailoring treatment to your cardiovascular profile enhances efficacy, ensuring optimal health outcomes. Always prioritize open communication with your doctor to determine the best course of action for your specific circumstances.
- 325 Aspirin Instead of Plavix: An In-Depth Analysis
- Comparative Effectiveness and Safety
- Patient Considerations
- Understanding the Mechanism of Action of Aspirin and Plavix
- Aspirin’s Mechanism of Action
- Plavix’s Mechanism of Action
- Clinical Considerations for Using 325 Aspirin as an Alternative
- Indications
- Dosing Considerations
- Monitoring and Follow-Up
- Comparative Efficacy and Safety Profiles of Aspirin and Plavix
325 Aspirin Instead of Plavix: An In-Depth Analysis
Switching to 325 mg of aspirin can provide adequate antiplatelet effects for patients who may benefit from an alternative to Plavix (clopidogrel). Aspirin effectively reduces the risk of cardiovascular events by inhibiting platelet aggregation, making it a reliable choice for many individuals.
Clinical studies indicate that higher doses of aspirin, such as 325 mg, can achieve a significant reduction in thrombotic complications. This dosage is particularly useful for patients with a history of acute coronary syndrome or those undergoing certain cardiovascular interventions. Patients should, however, consult with their healthcare providers to tailor the dosage based on their specific medical conditions and risk factors.
Comparative Effectiveness and Safety
Aspirin shows comparable effectiveness in preventing major cardiovascular events when compared to Plavix. In some cases, particularly in patients with aspirin resistance or those at high risk for gastrointestinal bleeding, Plavix might still be more appropriate. A healthcare professional can assess these risks and benefits, ensuring an informed decision is made.
Gastrointestinal side effects can occur with both medications. Monitoring for signs of bleeding is crucial, especially when taking higher doses of aspirin. Patients should report any unusual symptoms, such as black stool or persistent abdominal pain, to their doctors.
Patient Considerations
The choice between 325 mg of aspirin and Plavix hinges on individual health profiles, compliance, and potential drug interactions. Patients who have had prior adverse reactions to Plavix, or those seeking a less expensive alternative, might find aspirin to be a viable choice. Additionally, for individuals already on aspirin therapy, increasing the dosage may simplify treatment without the need for transitioning to a new medication.
In conclusion, 325 mg of aspirin may serve as a practical alternative to Plavix for certain patients. Continuous dialogue with healthcare providers ensures optimal management and adjustments based on patient needs. Regular follow-ups play a significant role in assessing the effectiveness and safety of the chosen antiplatelet therapy.
Understanding the Mechanism of Action of Aspirin and Plavix
Aspirin and Plavix (clopidogrel) serve critical roles in preventing cardiovascular events, but they operate through different biochemical avenues. Both drugs inhibit platelet aggregation, yet their pathways differ significantly.
Aspirin’s Mechanism of Action
Aspirin functions primarily by irreversibly inhibiting the enzyme cyclooxygenase (COX). This inhibition decreases the synthesis of thromboxane A2, a potent promoter of platelet activation and aggregation. As a result, aspirin effectively reduces the formation of blood clots. The action lasts for the lifetime of the platelet, approximately 7-10 days, making daily low-dose aspirin a common recommendation for individuals at risk of heart attacks and strokes.
Plavix’s Mechanism of Action
In contrast, Plavix works by blocking the P2Y12 receptor on platelets. This action prevents adenosine diphosphate (ADP) from activating the receptor, which is crucial for platelet activation and aggregation. Unlike aspirin, the inhibition by Plavix is not permanent and requires loading doses followed by maintenance doses to achieve effective platelet suppression. This makes Plavix particularly beneficial in scenarios like the prevention of thrombotic events after stent placement.
Both medications are pivotal in cardiovascular prevention strategies. Choice between them often depends on individual patient profiles, including risk factors and potential drug interactions. It is essential to consult healthcare providers to determine the most appropriate therapy for specific conditions.
Clinical Considerations for Using 325 Aspirin as an Alternative
Using 325 mg of aspirin as an alternative to Plavix (clopidogrel) can benefit patients requiring antiplatelet therapy. This approach may be appropriate for those with a history of gastrointestinal bleeding or other contraindications to newer antiplatelet agents.
Indications
- Patients with a history of acute coronary syndrome (ACS).
- Individuals undergoing percutaneous coronary intervention (PCI) who exhibit aspirin tolerance.
- Patients at increased risk of thrombotic events without major bleeding risks.
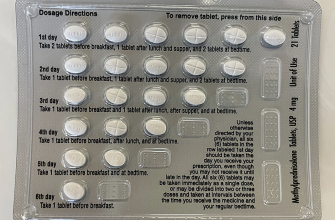
Dosing Considerations
The standard dose of 325 mg daily may need adjustment based on individual response and tolerance. It’s essential to monitor for potential side effects such as gastrointestinal discomfort or bleeding.
Start with the lowest effective dose and gradually increase if necessary, while always considering the patient’s complete medical history and concurrent medications.
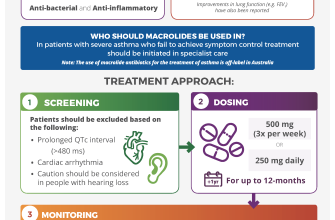
Monitoring and Follow-Up
- Regular evaluation of renal and hepatic function.
- Assessment for any signs of gastrointestinal bleeding.
- Counsel patients on recognizing symptoms of adverse reactions.
Patient education plays a crucial role. Inform patients about the importance of adhering to the prescribed regimen, potential interactions, and lifestyle modifications that may further reduce cardiovascular risk.
Overall, 325 mg of aspirin can serve as a practical alternative to Plavix in specific patient groups while ensuring vigilant monitoring and individualized care strategy.
Comparative Efficacy and Safety Profiles of Aspirin and Plavix
Aspirin demonstrates similar antiplatelet effects when compared to Plavix, particularly in patients at risk of cardiovascular events. Clinical studies have shown that a daily dose of 325 mg of aspirin can reduce the incidence of heart attacks and strokes effectively, making it a straightforward option for many. In various trials, the efficacy of aspirin alone was often comparable to that of Plavix, especially in patients with stable coronary artery disease.
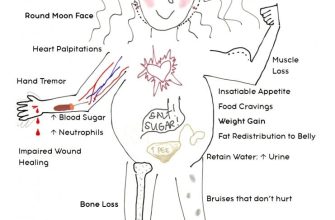
Safety profiles vary significantly. Aspirin commonly leads to gastrointestinal issues, such as irritation or bleeding, particularly in older populations or those with a history of ulcers. Conversely, Plavix tends to have a lower incidence of gastrointestinal complications. However, Plavix may lead to a different risk landscape, including bleeding events, which are also crucial to monitor.
The choice between the two often comes down to individual patient risk factors. For patients with a higher risk of gastrointestinal bleeding, Plavix could present a safer alternative. However, aspirin remains a first-line treatment due to its cost-effectiveness and ease of accessibility. Such factors play a crucial role in therapy selection.
In summary, both medications have their place in therapy. Assessing a patient’s specific risks and benefits will help decide which antiplatelet agent offers the best protection against vascular events. Regular follow-ups and monitoring for side effects will ensure safety while maximizing efficacy.