Monitor patients on amiodarone for ocular toxicity to prevent serious complications. Regular eye examinations are vital to detect any early signs of toxicity, especially in those taking high doses or on long-term therapy. Milder symptoms, such as blurred vision or halos around lights, may indicate corneal deposits, which can progress if untreated.
Educate patients about the potential visual disturbances associated with amiodarone. Encourage them to report any changes, as early intervention can lead to better outcomes. Symptoms might include photophobia, dryness, or peripheral vision changes. In some cases, these issues may resolve with dose adjustments or substitution with alternative medications.
Be aware of the potential for more serious conditions, such as optic neuropathy, which can lead to permanent vision loss if ignored. Regular follow-ups and prompt referrals to ophthalmologists for any severe symptoms ensure timely management of amiodarone-related ocular effects. Maintaining open lines of communication with your patients will help address their concerns effectively.
- Amiodarone Ocular Toxicity
- Understanding Amiodarone and Its Uses
- Key Indications for Amiodarone
- Administration and Dosage Guidelines
- Mechanism of Ocular Toxicity Induced by Amiodarone
- Clinical Manifestations of Amiodarone-Related Eye Damage
- Corneal Deposits
- Visual Disturbances and Optic Neuropathy
- Risk Factors for Developing Ocular Toxicity from Amiodarone
- Duration and Dosage of Amiodarone Therapy
- Concurrent Medications and Health Conditions
- Diagnostic Approaches for Identifying Ocular Toxicity
- Management and Treatment Options for Amiodarone-Induced Ocular Toxicity
Amiodarone Ocular Toxicity
Monitor patients on amiodarone regularly for ocular toxicity, particularly after long-term use. Patients may experience corneal deposits, which are common and often harmless but can lead to symptoms like glare and vision disturbances.
Conduct a thorough eye examination, including slit-lamp evaluation, to assess the extent of corneal deposits. Advise patients to report any changes in vision or discomfort promptly. Encourage regular follow-ups with an ophthalmologist, especially for those experiencing significant symptoms.
Educate patients about potential visual side effects, emphasizing awareness of their symptoms. Discuss the possible need for dosage adjustments or alternative therapies if ocular toxicity becomes troublesome.
Consider additional factors such as concomitant medications that might exacerbate ocular side effects. Patients with pre-existing ocular conditions should be monitored closely. Ensure they understand the importance of adhering to ophthalmologic care to prevent complications.
Understanding Amiodarone and Its Uses
Amiodarone is primarily utilized in the treatment of various tachyarrhythmias, including atrial fibrillation and ventricular tachycardia. Its effectiveness stems from its ability to prolong the action potential and refractory period in cardiac tissue, which stabilizes heart rhythms. This antiarrhythmic medication acts on multiple ion channels and possesses both beta-blocking and calcium channel-blocking properties, contributing to its versatile use in cardiology.
Key Indications for Amiodarone
Healthcare providers prescribe amiodarone for patients who experience life-threatening ventricular arrhythmias. It also serves as a long-term management option for atrial fibrillation, particularly in patients where alternatives are ineffective or contraindicated. Furthermore, it is valuable in patients with heart failure who may have an increased risk of arrhythmias.
Administration and Dosage Guidelines
Amiodarone is available in oral and intravenous formulations. For acute situations, intravenous administration allows rapid therapeutic effects. Dosage adjustments are often necessary based on individual patient response and side effects. Regular monitoring is essential to assess for potential adverse effects, especially with long-term oral use.
Maintain open communication with your healthcare team regarding any side effects experienced while on amiodarone. Early detection of complications, including ocular toxicity, significantly improves management outcomes.
Mechanism of Ocular Toxicity Induced by Amiodarone
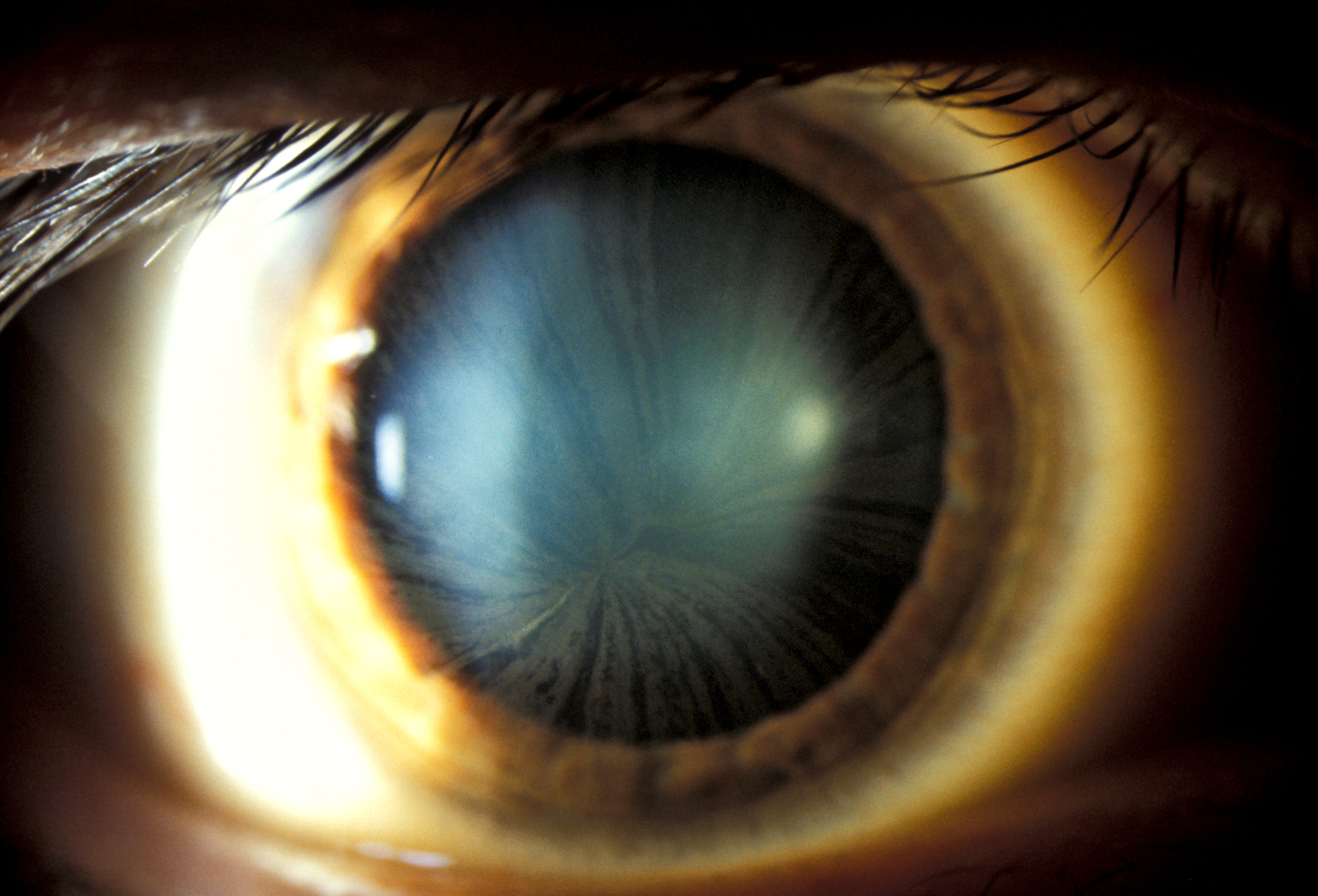
Amiodarone induces ocular toxicity primarily through its interaction with retinal cells and the deposition of metabolites. It alters cellular membranes, impacts lipid metabolism, and creates oxidative stress, resulting in cellular damage.
The drug’s high lipid solubility enables it to accumulate in tissues, particularly in the cornea and retina. Accumulation leads to the formation of deposits, which can disrupt normal visual function. The corneal epithelium displays corneal deposits, often manifesting as microdeposits, contributing to blurriness and decreased vision.
Oxidative stress plays a significant role in amiodarone-induced damage. It generates reactive oxygen species (ROS), leading to inflammation and apoptosis of retinal cells. These effects are linked to mitochondrial dysfunction, exacerbating visual impairment.
Furthermore, amiodarone affects the blood-retinal barrier. Changes in endothelial permeability can lead to edema and retinal hemorrhages, compounding visual complications. This barrier disruption facilitates inflammatory cell migration, perpetuating ocular toxicity.
Regular monitoring of ocular health in patients on amiodarone therapy is essential. Early detection of ocular toxicity allows for timely management, potentially preventing irreversible damage. Consider routine ophthalmic examinations for at-risk individuals to assess corneal and retinal health.
Clinical Manifestations of Amiodarone-Related Eye Damage
Regular monitoring of patients on amiodarone treatment is crucial due to potential ocular toxicity. Clinicians should remain vigilant for various eye symptoms that may indicate damage. The most common manifestations include corneal deposits, visual disturbances, and optic neuropathy.
Corneal Deposits
Corneal deposits often appear as a result of amiodarone use. These deposits typically present as asymptomatic, golden-brown or grayish-yellow opacities in the corneal epithelium. Examination under slit-lamp can reveal these deposits, primarily located at the limbus. They do not usually affect visual acuity but may lead to complaints of glare or visual blurring in some patients.
Visual Disturbances and Optic Neuropathy
Patients might experience visual disturbances, including blurred vision, halos around lights, or changes in color perception. This occurs due to the interaction of amiodarone with retinal structures. In rare cases, optic neuropathy may develop, leading to more significant vision loss. Prompt identification and management are essential to prevent irreversible damage.
| Manifestation | Characteristics | Recommendation |
|---|---|---|
| Corneal Deposits | Asymptomatic; golden-brown opacities | Regular slit-lamp examinations; no treatment needed |
| Visual Disturbances | Blurring; halos; color perception changes | Monitor symptoms; consider referral to specialist if persistent |
| Optic Neuropathy | Significant vision loss | Urgent ophthalmologic evaluation; possible medication review |
Awareness of these clinical manifestations is essential for timely intervention. Regular assessments and patient education can help manage the risks associated with amiodarone therapy while optimizing treatment outcomes.
Risk Factors for Developing Ocular Toxicity from Amiodarone
Patients utilizing amiodarone should be aware of several risk factors that can increase the likelihood of developing ocular toxicity. Older age stands out as a significant contributor, as the ocular structure naturally undergoes changes over time, making the eyes more vulnerable to drug-related effects. Additionally, individuals with pre-existing ocular conditions, such as corneal endothelial dystrophies or retinal disorders, may experience worsened outcomes due to amiodarone’s impact on ocular tissues.
Duration and Dosage of Amiodarone Therapy
Long-term therapy and higher cumulative doses of amiodarone elevate the risk of ocular complications. Prior studies indicate a linear correlation between dosage and the incidence of corneal deposits, which can lead to visual disturbances. Monitoring these factors closely can help mitigate potential toxicity.
Concurrent Medications and Health Conditions
Co-administration of other medications that may also affect ocular health, such as certain diuretics and antihypertensives, can compound the risk. Patients with systemic diseases like thyroid disorders or hyperlipidemia might also be at greater risk, as these conditions can influence drug metabolism and ocular responsiveness. Regular eye examinations become vital in the management of patients on long-term amiodarone therapy.
Diagnostic Approaches for Identifying Ocular Toxicity
Perform a thorough patient history assessment, focusing on medication use, duration of amiodarone treatment, and any ocular symptoms experienced. Inquire specifically about visual disturbances, color vision changes, or symptoms like dry eyes and discomfort.
Conduct a comprehensive eye examination. Start with visual acuity tests to assess any impact on vision. Follow this with a slit-lamp examination, facilitating the observation of corneal deposits and other morphological changes in the eye.
Utilize fundoscopy to examine the retina. Look for specific changes such as retinal pigmentary alterations, which may indicate toxicity. Evaluate the optic disc for signs of swelling or other anomalies.
Implement specific diagnostic imaging techniques if necessary. Optical coherence tomography (OCT) can provide detailed images of the retina, helping to identify any layers that may be affected by amiodarone toxicity.
Consider performing visual field tests to detect peripheral vision changes. This can reveal subtle disturbances that may not be initially apparent during routine examinations.
Order color vision tests, as amiodarone can affect this aspect of sight. The Ishihara test remains a standard method for assessing color discrimination.
If ocular toxicity is suspected, conduct an assessment of corneal sensitivity. This may involve using a cotton wisp or other standardized methods to quantify any sensory alterations.
Finally, collaborate with an ophthalmologist for advanced diagnostics or if the patient exhibits severe symptoms. Their expertise lies in managing ocular complications and can provide additional insights into treatment options.
Management and Treatment Options for Amiodarone-Induced Ocular Toxicity
Discontinue amiodarone therapy immediately upon diagnosis of ocular toxicity. Consult an ophthalmologist for a comprehensive eye examination to assess the extent of damage.
Follow these management strategies:
- Regular Monitoring: Schedule frequent eye exams to monitor progression or improvement of symptoms.
- Topical Therapies: Prescribe artificial tears to alleviate dryness and irritation. Consider corticosteroids for inflammation after evaluating risks versus benefits.
- Antioxidants: Introduce antioxidant supplements such as vitamin E and C, which may provide additional protection against oxidative stress in ocular tissues.
- Referral to Specialists: In cases of severe toxicity, refer patients to a retinal specialist for potential interventions like laser treatments or vitrectomy.
Educate patients about the symptoms of ocular toxicity. Instruct them to report any visual disturbances promptly, as early intervention can significantly impact outcomes.
Encourage routine follow-ups after cessation of therapy to assess for any delayed effects. Document changes in vision and other ocular symptoms meticulously.
Consider alternative antiarrhythmic medications if amiodarone is no longer viable, weighing the patient’s cardiac condition against the risk of ocular side effects associated with these alternatives.
Promote lifestyle modifications that benefit ocular health, such as wearing sunglasses to reduce UV exposure and maintaining adequate hydration.