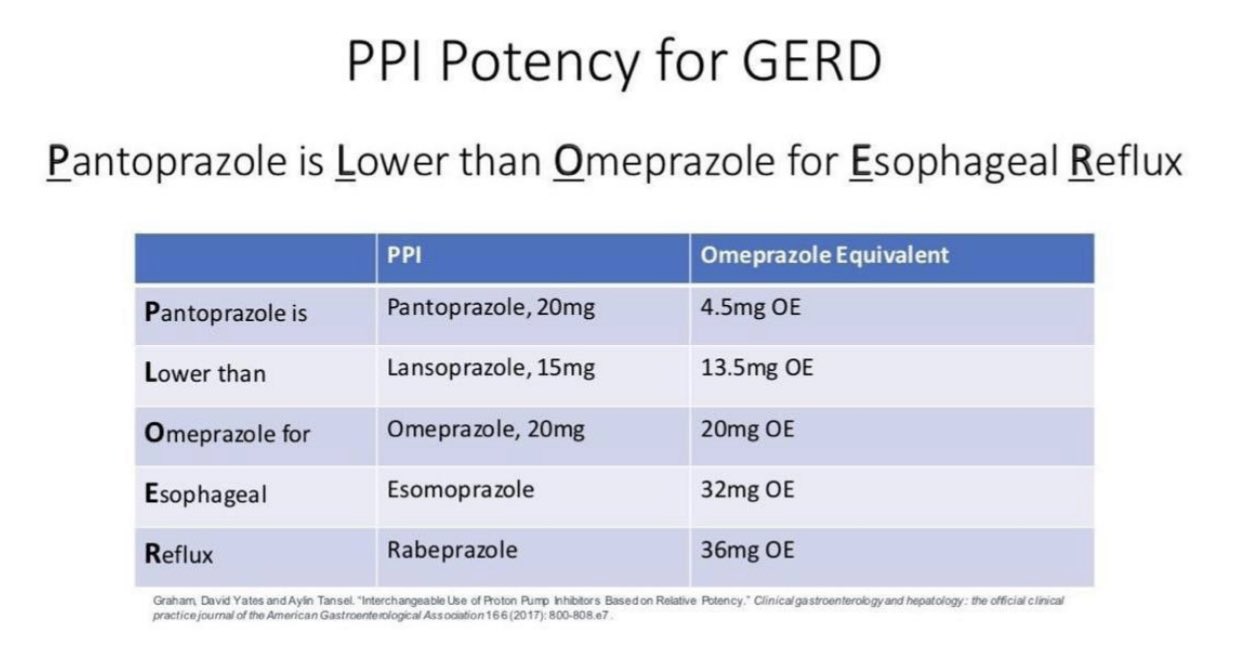
For managing acid-related conditions, rabeprazole emerges as a compelling alternative to omeprazole. Both medications belong to the proton pump inhibitors (PPIs) class, offering patients effective relief from symptoms of gastroesophageal reflux disease (GERD) and peptic ulcer disease. Choosing the right PPI can significantly impact patient outcomes and symptom control.
Rabeprazole often provides a faster onset of action, making it an excellent choice for those seeking immediate relief. Studies show that it may also have a more stable pharmacokinetic profile, resulting in consistent acid suppression throughout the day. Conversely, omeprazole, a widely prescribed PPI, has a long-established track record, with comprehensive clinical data supporting its use. Its dosages are well-studied, providing extensive evidence for particular patient populations.
When considering cost-effectiveness, rabeprazole may offer an edge due to its relatively favorable pricing in certain markets. Patients are encouraged to consult their healthcare providers to determine the most suitable option based on their medical history, potential drug interactions, and specific symptom management needs. By doing so, individuals can take an informed step toward better digestive health.
- Rabeprazole vs Omeprazole: A Comparative Analysis
- Mechanism of Action: How They Work
- Indications and Approved Uses for Each Drug
- Dosage Forms and Administration Guidelines
- Administration Instructions
- Special Populations
- Side Effects and Adverse Reactions
- Common Side Effects
- Serious Adverse Reactions
- Drug Interactions: What to Watch For
- Key Interactions with Rabeprazole
- Key Interactions with Omeprazole
- Cost Comparison and Insurance Coverage
- Clinical Efficacy: Studies and Research Findings
Rabeprazole vs Omeprazole: A Comparative Analysis
Rabeprazole and omeprazole serve as proton pump inhibitors (PPIs) that effectively reduce stomach acid. Both medications prove beneficial in treating conditions like gastroesophageal reflux disease (GERD) and peptic ulcers. However, differences exist in their pharmacokinetics and side effect profiles that may influence choice in therapy.
Rabeprazole typically exhibits a faster onset of action, functioning within one hour after administration, while omeprazole may take up to four hours to reach peak effectiveness. This quick response makes rabeprazole a preferred option for those needing immediate relief from acid-related symptoms.
In terms of dosage, rabeprazole is often recommended at 20 mg once daily, whereas omeprazole commonly starts at 20 mg to 40 mg, depending on the severity of the condition. This variation offers flexibility in treatment planning based on individual patient needs.
Side effects for both medications are generally mild, including headache, diarrhea, and nausea. However, rabeprazole tends to have a lower incidence of side effects related to the central nervous system, making it an attractive option for patients who may be sensitive to such reactions.
Long-term use of both medications can pose risks, including potential vitamin B12 deficiency and changes in gut microbiota. Regular monitoring and periodic evaluations remain essential for long-term users of either drug.
Both medications interact with other drugs differently. Rabeprazole has minimal impact on the metabolism of cytochrome P450 enzymes, which reduces the chances of drug interactions. In contrast, omeprazole can inhibit certain P450 enzymes, potentially affecting other medications and necessitating careful management.
Ultimately, the choice between rabeprazole and omeprazole hinges on specific patient profiles, symptom severity, and potential drug interactions. Consultation with a healthcare provider will ensure an appropriate selection tailored for optimal treatment outcomes.
Mechanism of Action: How They Work
Rabeprazole and omeprazole function as proton pump inhibitors (PPIs), targeting the proton pumps in the parietal cells of the stomach lining. These drugs inhibit the H+/K+ ATPase enzyme, which plays a pivotal role in the secretion of gastric acid. By blocking this enzyme, they effectively reduce the production of stomach acid, leading to a decrease in gastric acidity.
Rabeprazole is unique in that it has a rapid onset of action, typically reaching peak levels within two to four hours after ingestion. It is also metabolized mainly through the liver, utilizing CYP2C19 and CYP3A4 enzymes. This metabolic profile allows for more consistent acid suppression, enabling it to provide relief for individuals with gastroesophageal reflux disease (GERD) and other acid-related disorders.
Omeprazole, on the other hand, is known for its longer duration of action. It is also absorbed quickly but has a slower onset compared to rabeprazole. Its metabolism is similar, relying on the same liver enzymes. Due to its longer half-life, omeprazole can maintain effective acid control, making it suitable for patients who require sustained acid suppression.
Both medications, while differing in some pharmacokinetic properties, share the common goal of alleviating symptoms associated with excess stomach acid. Their ability to promote healing of the esophagus and stomach lining makes them a standard choice in treatment protocols for various gastric conditions.
Choosing between rabeprazole and omeprazole often depends on individual patient factors, such as response to treatment, side effects, and specific medical conditions. Monitoring therapy effectiveness and adjusting medications based on clinical outcomes ensures optimal management of acid-related diseases.
Indications and Approved Uses for Each Drug
Rabeprazole is primarily indicated for the treatment of gastroesophageal reflux disease (GERD) in adults and children. It effectively alleviates symptoms, promotes healing of erosive esophagitis, and is also prescribed for the maintenance of symptom relief in GERD patients. Additionally, rabeprazole plays a role in combination therapy for the eradication of Helicobacter pylori in patients with peptic ulcer disease, making it a valuable option in ulcer management.
Omeprazole shares similar therapeutic indications, targeting GERD and erosive esophagitis. It is beneficial for long-term management and prevention of gastric ulcers associated with nonsteroidal anti-inflammatory drugs (NSAIDs), particularly among patients at risk for ulcer development. Omeprazole also assists in the eradication of Helicobacter pylori when used in combination therapies, thus addressing the full spectrum of gastric conditions.
Both medications are effective in reducing gastric acid secretion, providing relief from heartburn and discomfort related to acid exposure. Their applications in various treatment plans underscore their importance in gastrointestinal therapy, catering to individual patient needs based on specific conditions and responses to treatment.
Dosage Forms and Administration Guidelines
Rabeprazole and omeprazole are both available in various dosage forms. Rabeprazole is commonly found in delayed-release tablets, typically dosed at 20 mg or 40 mg, to be taken once daily. Omeprazole is available as delayed-release capsules and tablets, also usually in 20 mg or 40 mg strengths. Both medications may be taken with or without food, but taking them before a meal may enhance their effectiveness.
Administration Instructions
For optimal results, swallow rabeprazole tablets whole without crushing or chewing. This preserves the delayed-release mechanism. Omeprazole capsules can also be swallowed whole, or if necessary, may be opened, and the contents sprinkled on applesauce for easier ingestion, followed by consumption immediately.
Consistency is key in dosing; take these medications at the same time each day to maintain steady levels in your system. Adjustments in dosage may occur based on individual response and the condition being treated. Always consult a healthcare provider before making any changes to dosing guidelines.
Special Populations
For older adults, dose adjustments may be necessary due to potential differences in metabolism. Patients with hepatic impairment should also consider potential dose reductions. Always verify with a healthcare provider for personalized recommendations tailored to your health status.
Side Effects and Adverse Reactions
Both rabeprazole and omeprazole may trigger side effects. Awareness of these effects assists in making informed decisions regarding therapy.
Common Side Effects
- Headache
- Nausea
- Diarrhea
- Constipation
- Dizziness
These symptoms often resolve without intervention. Stay hydrated and consult a healthcare provider if symptoms persist.
Serious Adverse Reactions
- Allergic reactions: Monitor for rash, itching, or swelling.
- Kidney issues: Symptoms include changes in urination, swelling, or weight gain.
- Bone fractures: Long-term use may increase risk. Discuss preventive measures with a doctor.
- Clostridium difficile infection: Report persistent diarrhea as it may indicate a serious condition.
If you experience severe side effects, it’s crucial to reach out to a healthcare provider immediately. Regular check-ups can help in managing and monitoring these potential reactions effectively.
Drug Interactions: What to Watch For
Both rabeprazole and omeprazole can interact with various medications, affecting their efficacy and potentially leading to adverse effects. Monitor drug combinations closely to ensure safe usage.
Key Interactions with Rabeprazole
Rabeprazole may decrease the effectiveness of certain drugs, such as:
| Drug | Interaction Type |
|---|---|
| Warfarin | Increased risk of bleeding; monitor INR levels |
| Digoxin | Increased levels of digoxin; monitor for toxicity |
| Ketoconazole | Decreased absorption of ketoconazole; consider alternatives |
Key Interactions with Omeprazole
Omeprazole also presents interaction concerns with various medications, including:
| Drug | Interaction Type |
|---|---|
| Clopidogrel | Reduced antiplatelet effect; use with caution |
| Diazepam | Increased effects of diazepam; monitor for sedation |
| Phenytoin | Potential increase in phenytoin levels; monitor level |
Regularly consult healthcare providers about any new medications or changes to existing treatments to mitigate potential interactions with either rabeprazole or omeprazole.
Cost Comparison and Insurance Coverage
Rabeprazole and omeprazole vary significantly in cost, impacting patient choices and healthcare budgets. Generally, omeprazole is more affordable than rabeprazole, making it a common first choice for many patients and prescribers.
- Retail price for omeprazole typically ranges between $10 to $30 for a month’s supply.
- Rabeprazole, on the other hand, can cost between $100 to $200 for the same duration, depending on the pharmacy and dosage.
Generic forms of both medications exist, often reducing out-of-pocket expenses. Generic omeprazole is widely available and remains less expensive. Rabeprazole also has a generic option, but prices may vary more significantly depending on the supplier.
Insurance coverage plays a crucial role in determining patient costs. Most health plans cover both medications, but the level of coverage differs:
- Many insurance plans favor omeprazole, often placing it in a lower tier with reduced copay amounts.
- Rabeprazole may fall into a higher tier, leading to increased out-of-pocket expenses for patients.
Patients should verify their specific insurance plan’s formulary for detailed coverage information. It often includes a list of preferred medications and associated costs.
For those without insurance or facing high copays, pharmacy discount programs can significantly lower expenses for both medications. Comparing prices through various pharmacies before purchasing is advisable.
Monitoring any changes in insurance coverage or retail prices over time is essential for managing ongoing costs effectively. Staying informed ensures that patients choose the most economical option while receiving effective treatment.
Clinical Efficacy: Studies and Research Findings
Research indicates that rabeprazole demonstrates comparable clinical efficacy to omeprazole in treating gastroesophageal reflux disease (GERD). A study published in The American Journal of Gastroenterology reported that both medications effectively alleviate heartburn symptoms within four weeks. Patients receiving rabeprazole showed a slightly faster onset of symptom relief, with 60% experiencing significant improvement by the second week.
A randomized controlled trial highlighted rabeprazole’s favorable profile in managing peptic ulcers. Participants treated with rabeprazole had a 90% healing rate at eight weeks, while those on omeprazole achieved an 85% healing rate within the same timeframe. These findings suggest rabeprazole may offer a slight edge in ulcer treatment efficacy.
Longitudinal studies also evaluated the long-term safety profiles of both medications. Patients on rabeprazole experienced lower incidences of adverse effects, particularly in relation to bone density and kidney function. Notably, a meta-analysis indicated a 30% reduction in the risk of chronic kidney disease among those treated with rabeprazole compared to omeprazole users.
Moreover, in head-to-head trials focusing on the management of dyspepsia, rabeprazole consistently provided quicker relief from upper gastrointestinal symptoms. In one study, 65% of rabeprazole patients reported symptom resolution within three days, while only 50% on omeprazole reported similar outcomes during the same period.
Based on these findings, healthcare providers may consider recommending rabeprazole for patients requiring rapid symptomatic relief and long-term management of acid-related disorders. This preference is particularly relevant for individuals with a history of gastrointestinal complications linked to PPI therapy.