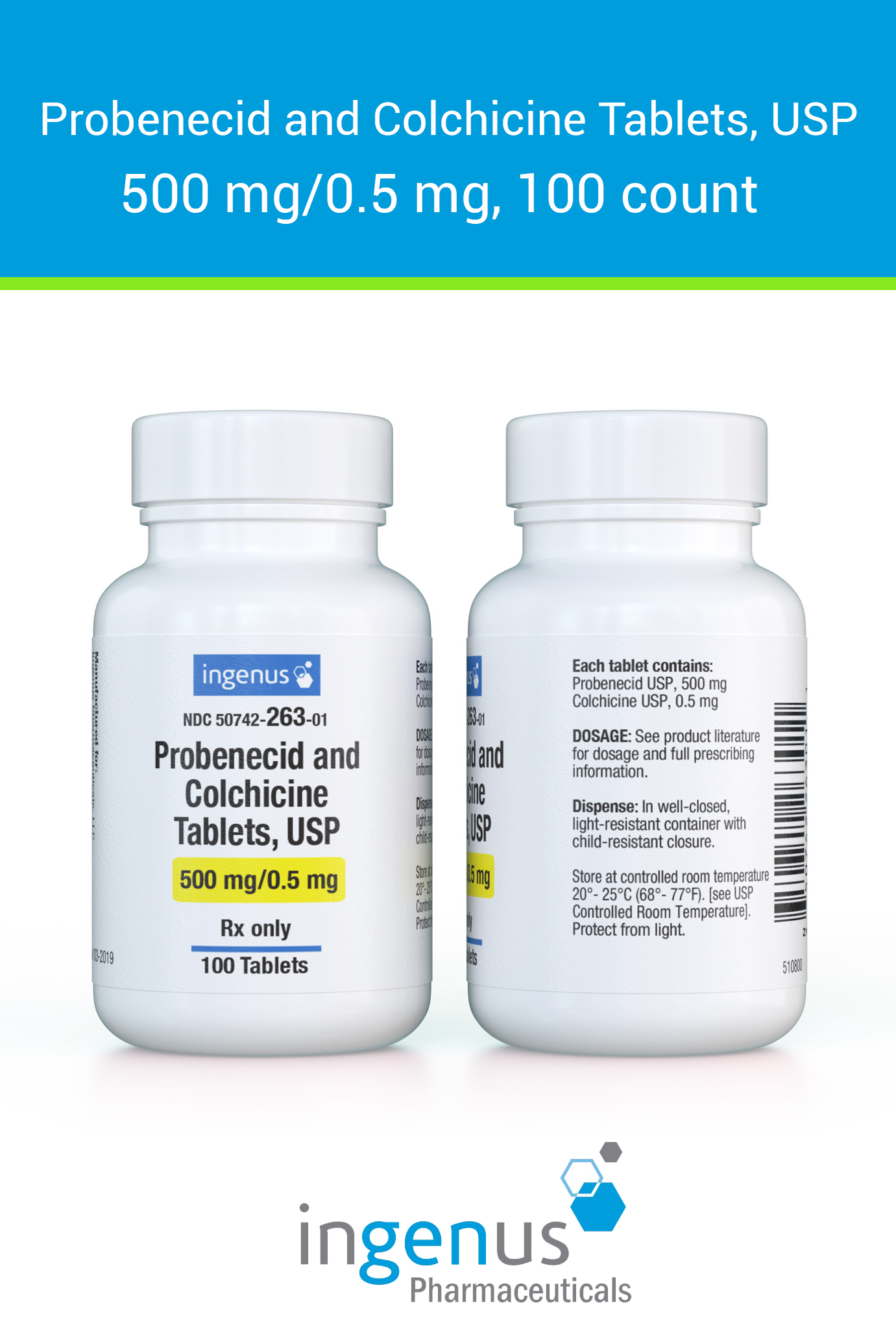
Consider incorporating Probenecid and Colchicine into your treatment plan for managing gout flare-ups effectively. These two medications work synergistically to reduce symptoms and prevent future attacks. Probenecid promotes the excretion of uric acid, lowering its levels in the body, while Colchicine addresses inflammation associated with gout attacks.
When starting Probenecid, aim for a dosage of 500 mg once a day, gradually increasing as needed, under medical supervision. This gradual increase helps to minimize potential side effects. Pairing this with Colchicine, particularly during acute attacks, can significantly enhance relief. A typical regimen includes a loading dose of Colchicine, followed by a lower dose to prevent recurrence.
Monitor renal function and uric acid levels regularly to ensure optimal medication efficacy and safety. By tailoring treatment, you can maintain better control over gout and enhance your quality of life. Always discuss your plan with a healthcare provider to personalize dosages and combinations that best suit your needs.
- Probenecid Colchicine: A Comprehensive Overview
- Dosage and Administration
- Potential Side Effects
- Mechanism of Action and Pharmacokinetics of Probenecid and Colchicine
- Probenecid Mechanism of Action
- Colchicine Mechanism of Action
- Pharmacokinetics of Probenecid
- Pharmacokinetics of Colchicine
- Clinical Indications and Patient Selection for Probenecid and Colchicine Therapy
- Patient Eligibility Criteria
- Monitoring and Follow-Up
- Potential Side Effects and Drug Interactions with Probenecid and Colchicine
- Drug Interactions
- Recommendations
Probenecid Colchicine: A Comprehensive Overview
Probenecid colchicine is a therapeutic option for managing gout flares and chronic gouty arthritis. This combination effectively reduces serum uric acid levels while alleviating inflammation. Probenecid works by inhibiting renal tubular reabsorption of uric acid, promoting its excretion, which is essential for lowering uric acid levels in the body. Colchicine complements this effect by targeting inflammation directly, providing pain relief during acute attacks.
Dosage and Administration
The typical starting dose for probenecid is 250 mg twice daily, which can be gradually increased. It’s important to maintain hydration and monitor renal function during treatment. For colchicine, the recommended dosage is 1.2 mg at the first sign of a flare, followed by 0.6 mg one hour later. This regimen helps control pain and discomfort effectively. Adjustments may be necessary based on individual response and tolerance.
Potential Side Effects
While probenecid colchicine is generally well-tolerated, some patients may experience gastrointestinal disturbances such as nausea or diarrhea. Allergic reactions, albeit rare, require immediate medical attention. Persistent headache or dizziness can occur; patients should discuss these symptoms with their healthcare provider. Regular follow-ups can help manage any adverse reactions effectively.
Mechanism of Action and Pharmacokinetics of Probenecid and Colchicine
Probenecid and colchicine operate through distinct yet complementary mechanisms, enhancing treatment strategies for conditions like gout.
Probenecid Mechanism of Action
Probenecid primarily inhibits renal tubular reabsorption of uric acid. By blocking the urate transporter (URAT1), it promotes increased uric acid excretion, effectively lowering serum urate levels. Additionally, probenecid enhances the plasma levels of certain antibiotics, such as penicillin, by inhibiting their renal excretion.
Colchicine Mechanism of Action
Colchicine targets microtubule formation, disrupting the inflammatory response in gout. It inhibits neutrophil migration to inflamed tissues and decreases the release of inflammatory mediators. This action alleviates acute gout attacks and reduces the frequency of flare-ups in chronic conditions.
Pharmacokinetics of Probenecid
- Absorption: Rapidly absorbed from the gastrointestinal tract, reaching peak plasma concentrations within 1-2 hours.
- Distribution: Widely distributed, highly protein-bound (95-99%), with a volume of distribution of approximately 0.5 L/kg.
- Metabolism: Undergoes minimal hepatic metabolism and is primarily excreted unchanged in urine.
- Half-life: Approximately 5-8 hours, allowing for once or twice daily dosing.
Pharmacokinetics of Colchicine
- Absorption: Rapidly absorbed following oral administration; onset of action typically occurs within 30-60 minutes.
- Distribution: Extensively distributed to tissues; moderately protein-bound (40-50%).
- Metabolism: Primarily metabolized by the liver, primarily via CYP3A4 enzymes; potential interactions with other medications.
- Half-life: About 9-16 hours, often requiring multiple doses to maintain therapeutic levels.
Combining probenecid and colchicine can enhance the effectiveness in managing gout. Regular monitoring of uric acid levels and adjustments in dosage may be necessary to achieve optimal results while minimizing side effects.
Clinical Indications and Patient Selection for Probenecid and Colchicine Therapy
Probenecid and colchicine therapy is particularly beneficial for patients with gout. It aims to decrease uric acid levels and prevent acute attacks through different mechanisms. Selected patients should have a confirmed diagnosis of chronic gout, characterized by recurrent flares or tophi formation. They must also have insufficient response or intolerance to first-line treatments.
Patient Eligibility Criteria
An ideal candidate for this combined therapy is someone with frequent acute gout attacks, defined as more than two episodes per year. Patients with chronic kidney disease (CKD) should be carefully evaluated. If renal function is stable and urate excretion is impaired, probenecid can effectively enhance urate clearance.
Colchicine is suitable for pain relief during an acute flare and as a preventive measure during the initiation of urate-lowering therapy. Patients at risk of gastrointestinal side effects may require dose adjustments or alternative medications. Caution is advised for those with hepatic or renal impairment.
Monitoring and Follow-Up
Regular monitoring of renal function and uric acid levels is necessary to assess therapy effectiveness and adjust dosages. Keeping track of side effects, especially gastrointestinal symptoms, ensures safety and treatment adherence. Engage patients in discussions about their experience with the medication, allowing timely interventions if issues arise.
In summary, this therapy is suited for gout patients with recurrent attacks, specific renal profiles, and who require enhancement of urate clearance. A tailored approach to individual patient needs will facilitate successful management of gout and improve quality of life.
Potential Side Effects and Drug Interactions with Probenecid and Colchicine
Monitoring for side effects when taking Probenecid and Colchicine is essential. Common side effects include gastrointestinal disturbances such as nausea, vomiting, and diarrhea. Skin reactions may occur, leading to rashes or itching. Some individuals may experience headaches or dizziness. If severe side effects develop, discontinue use and consult a healthcare professional.
Drug Interactions
Probenecid can influence the effectiveness of several medications by altering their absorption and elimination. It may increase the concentration of certain drugs, such as penicillins and cephalosporins, potentially enhancing their efficacy but also raising the risk of adverse effects. Combining Probenecid with methotrexate can elevate toxicity levels, leading to serious health concerns.
Colchicine must also be approached cautiously. Concurrent use with drugs that inhibit CYP3A4, like certain antifungals and macrolide antibiotics, can lead to increased colchicine levels, increasing the likelihood of toxicity. Always notify your healthcare provider of all medications being taken to adjust dosages as necessary.
Recommendations
Evaluate all medications and supplements with a healthcare provider before starting treatment with Probenecid and Colchicine. Regular monitoring of kidney function and blood counts is advisable to identify potential complications early. Keep a close watch for any unusual symptoms and report them immediately for timely intervention.