To address the growing concern of ciprofloxacin-resistant gonorrhea, healthcare providers must adopt targeted testing and treatment protocols. Regular screening for gonorrhea, especially in communities with high prevalence rates, is essential. Advance caution is advised: treatment with ciprofloxacin should be avoided in patients with confirmed or suspected infections, given the documented resistance patterns.
The Centers for Disease Control and Prevention (CDC) recommend using dual therapy with azithromycin and ceftriaxone as the first-line treatment. This combination addresses potential resistance and enhances treatment effectiveness. Healthcare professionals should stay updated on local resistance trends to tailor antibiotic choice appropriately.
Education on prevention strategies remains paramount. Promote the use of condoms and regular testing for sexually active individuals, particularly those with multiple partners. This proactive approach not only mitigates the spread of resistant strains but also promotes overall sexual health.
Monitoring and reporting resistance patterns will aid in refining treatment guidelines and improving patient outcomes. Collaboration among healthcare providers, patients, and public health officials is vital to combat this rising threat effectively.
- Cipro Resistant Gonorrhea: A Growing Public Health Concern
- Understanding the Mechanisms of Cipro Resistance in Gonorrhea
- Current Epidemiology of Cipro Resistant Gonorrhea Cases
- Geographic Distribution
- Clinical Recommendations
- Guidelines for Screening and Diagnosis in At-Risk Populations
- Treatment Options and Management for Cipro Resistant Gonorrhea
- Alternative Treatments
- Follow-Up and Management
- Preventive Strategies to Combat the Spread of Resistance
Cipro Resistant Gonorrhea: A Growing Public Health Concern
Cipro resistant gonorrhea presents significant challenges for treatment and control. Recent data indicates that resistance rates have increased globally, affecting traditional therapeutic approaches.
Testing for antibiotic resistance is crucial. Healthcare providers must utilize culture and sensitivity testing when treating suspected cases of gonorrhea. This ensures the chosen antibiotic remains effective against the resistant strains.
Incorporating dual therapy into treatment protocols is recommended. Using two antibiotics concurrently can help combat resistance and improve treatment outcomes. Currently, the CDC suggests combining ceftriaxone with azithromycin as a frontline approach.
Prompt identification and treatment of gonorrhea are vital to reduce the risk of complications and transmission. Regular screening in at-risk populations helps identify infections early. Healthcare systems should promote awareness and access to testing, especially in sexually active individuals.
Education on safe sex practices plays a pivotal role in prevention. Communities must be informed about the importance of barrier methods, such as condoms, to reduce transmission rates.
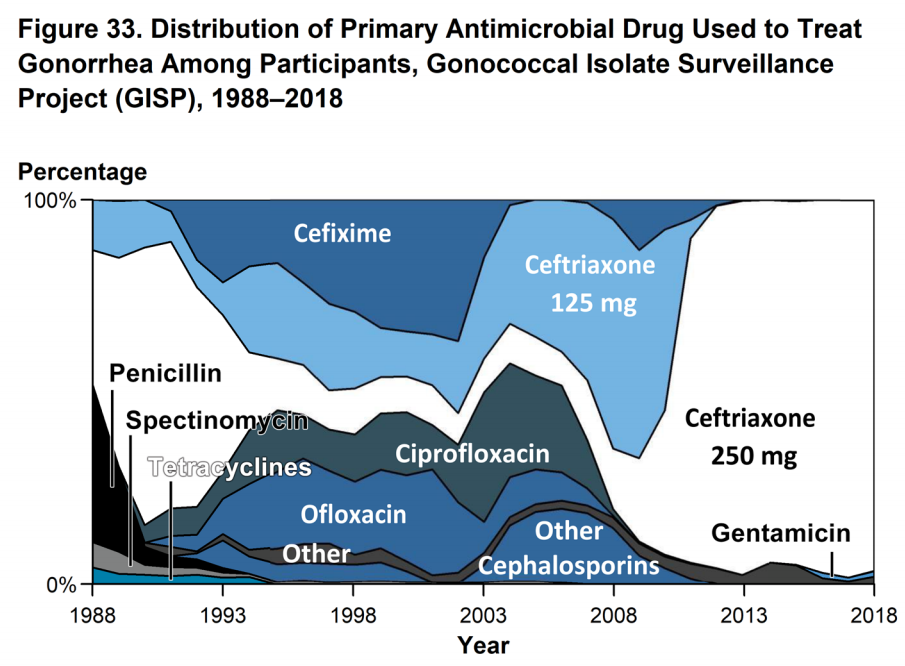
Public health initiatives should focus on monitoring antibiotic resistance patterns. Surveillance programs can provide critical insights into the effectiveness of treatment regimens and the development of resistance.
Lastly, ongoing research into alternative treatments is necessary. Exploring novel antibiotics and non-antibiotic therapies could offer new solutions in the fight against resistant gonorrhea strains.
Understanding the Mechanisms of Cipro Resistance in Gonorrhea
Ciprofloxacin resistance in Neisseria gonorrhoeae primarily arises from one central mechanism: genetic mutations. These mutations affect the target enzymes of the drug, specifically DNA gyrase and topoisomerase IV, which play critical roles in bacterial DNA replication and repair.
Mutations in the quinolone resistance-determining regions (QRDR) of these enzymes lead to changes in their structure, reducing the binding efficiency of ciprofloxacin. Studies have demonstrated that single nucleotide polymorphisms can significantly alter protein interactions, allowing the bacteria to replicate even in the presence of the antibiotic.
Another aspect contributing to resistance is the role of efflux pumps. These protein complexes help expel ciprofloxacin from the bacterial cell, lowering its intracellular concentration and minimizing its effectiveness. Genes that encode for these efflux pumps, when overexpressed, lead to heightened levels of resistance.
Environmental factors also influence resistance development. Overuse and misuse of antibiotics in both human medicine and agriculture create selective pressure, promoting the survival of resistant strains. Monitoring prescription practices and educating healthcare providers on appropriate use can curb this trend.
Furthermore, genetic exchange among bacteria, such as horizontal gene transfer, facilitates the spread of resistance genes. This inter-bacterial transfer occurs through plasmids or transposons, allowing non-resistant strains to acquire resistance characteristics rapidly.
Combating Cipro resistance requires a multi-faceted approach. Regular surveillance of resistance patterns in clinical settings helps inform treatment guidelines. Additionally, exploring alternative antibiotic options and developing new therapeutic strategies are crucial steps in managing infections caused by resistant strains of gonorrhea.
Ultimately, understanding these mechanisms equips healthcare professionals with the knowledge needed to address the rising challenge of Cipro-resistant gonorrhea effectively.
Current Epidemiology of Cipro Resistant Gonorrhea Cases
Ciprofloxacin resistance in gonorrhea remains a public health challenge. Recent data indicate an alarming increase in ciprofloxacin-resistant Neisseria gonorrhoeae strains across various regions. Surveillance reports from the Centers for Disease Control and Prevention (CDC) highlight that approximately 25% of gonorrhea cases in certain urban areas exhibit resistance to ciprofloxacin.
Emerging resistance patterns are particularly pronounced among men who have sex with men (MSM), with reports showing rates of ciprofloxacin resistance surpassing 30% in some populations. This demographic should follow testing protocols that include susceptibility testing, especially after unprotected intercourse with multiple partners.
Geographic Distribution
The highest prevalence of ciprofloxacin resistance is recorded in metropolitan settings. Large cities such as San Francisco, New York, and Seattle show pronounced resistance rates, often linked to high rates of transmission and inadequate access to effective treatments. States with lower overall sexually transmitted infection rates still report isolated outbreaks of resistant gonorrhea, emphasizing the need for vigilant monitoring in all areas.
Clinical Recommendations
Healthcare providers should prioritize dual therapy regimens, such as the combination of ceftriaxone and azithromycin, to mitigate treatment failures. Routine screening for gonorrhea in at-risk populations, particularly MSM and individuals with multiple sexual partners, plays a pivotal role in curtailing the spread of resistant strains. Timely intervention and updated treatment protocols will remain critical in the fight against ciprofloxacin-resistant gonorrhea.
Ongoing research into the mechanisms of resistance and the development of new antibiotics is essential. Collaboration between public health entities, healthcare providers, and communities will strengthen efforts to monitor, prevent, and treat resistant gonorrhea effectively.
Guidelines for Screening and Diagnosis in At-Risk Populations
Screening for gonorrhea, particularly in populations at risk for Cipro-resistant strains, should follow targeted recommendations. The Centers for Disease Control and Prevention (CDC) advises routine screening for sexually active individuals under 25 years and older populations with risk factors, such as multiple partners or a history of STIs.
Conduct tests at least annually, or more frequently–every three to six months–for those at heightened risk. Use nucleic acid amplification tests (NAATs) for accurate diagnosis, as they detect the genetic material of Neisseria gonorrhoeae effectively. Cultures may be necessary if antibiotic resistance is suspected.
The following table outlines screening recommendations based on risk factors:
| Population | Recommended Screening Frequency |
|---|---|
| Sexually active women under 25 | Annually |
| Men who have sex with men (MSM) | Every 3 to 6 months |
| Individuals with multiple sexual partners | Every 3 to 6 months |
| Pregnant women | First trimester and third trimester |
| Individuals with a history of STIs | Every 3 to 6 months |
Providers should educate patients on the importance of consistent screening and safe sexual practices. Encourage discussions around symptoms, even if they are mild or absent. Quick access to treatment following a positive diagnosis can prevent complications and spread within the community.
Review patient history for any antibiotic use prior to testing. This information assists in determining the appropriate testing method and potential need for culture testing to assess for resistance. Connect patients with resources for follow-up care and partner notification to help manage and control outbreaks effectively.
Treatment Options and Management for Cipro Resistant Gonorrhea
Utilize dual therapy as a primary strategy. The Centers for Disease Control and Prevention (CDC) recommend using ceftriaxone in combination with azithromycin to treat gonorrhea strains resistant to ciprofloxacin. Ensure that ceftriaxone is administered intramuscularly at a dose of 500 mg, while azithromycin can be given orally at 1 g.
Alternative Treatments
For patients with known allergies to the first-line options, consider the use of oral gemifloxacin or moxifloxacin. Both options are fluoroquinolones, but they often maintain effectiveness against Cipro-resistant strains. Use these alternatives cautiously, keeping in mind the specific resistance patterns in your region.
Follow-Up and Management
Schedule a follow-up appointment within one week after treatment to ensure the infection has cleared. Perform a test of cure using nucleic acid amplification tests (NAAT) to confirm the absence of the bacteria, especially for patients at high risk of infection. Patients with persistent symptoms despite treatment may require additional assessment and possibly alternative antibiotics.
- Ensure partners are also screened and treated for gonorrhea.
- Educate patients on prevention methods, including consistent condom use.
- Monitor for any adverse reactions to medications and manage accordingly.
Staying updated on local antibiotic resistance patterns will enhance treatment strategies. Engage with local health departments to access data and adjust protocols as necessary. Encourage patient engagement in their treatment journey to foster adherence and reduce reinfection risk.
Preventive Strategies to Combat the Spread of Resistance
Implement routine screenings for sexually transmitted infections (STIs), specifically for high-risk populations. Regular testing can catch infections early, preventing further transmission and complications related to drug resistance.
Encourage the use of safe sex practices, including consistent condom use. Providing education on proper condom usage can reduce the spread of gonorrhea and, subsequently, resistance formation.
Enhance public awareness campaigns that focus on the risks associated with untreated STIs. Informational sessions and workshops can address misconceptions, promote preventive measures, and empower individuals to seek prompt medical attention.
Advocate for judicious use of antibiotics. Healthcare providers should prescribe antibiotics based on sensitivity testing and avoid unnecessary prescriptions to reduce the chance of developing resistant strains.
Support collaboration between public health agencies and healthcare providers to establish a robust surveillance system. Monitoring resistance patterns helps in formulating informed treatment guidelines and tracking outbreaks promptly.
Empower individuals to take control of their sexual health by promoting accessible resources for information and health services. Clinics offering free or low-cost STI testing can encourage more people to seek care.
Engage in research to develop new treatment options and alternative therapies. Increased funding and support for studies focused on gonorrhea resistance can potentially lead to breakthroughs in managing this public health challenge.
Encourage open discussions about sexual health between partners. Promoting transparency regarding STI status can lead to proactive measures, such as testing and treatment, that limit transmission.
Lastly, advocate for policies that enhance access to healthcare. Ensuring that all individuals have the opportunity to receive medical care, regardless of socioeconomic status, is fundamental to controlling the spread of resistant gonorrhea.